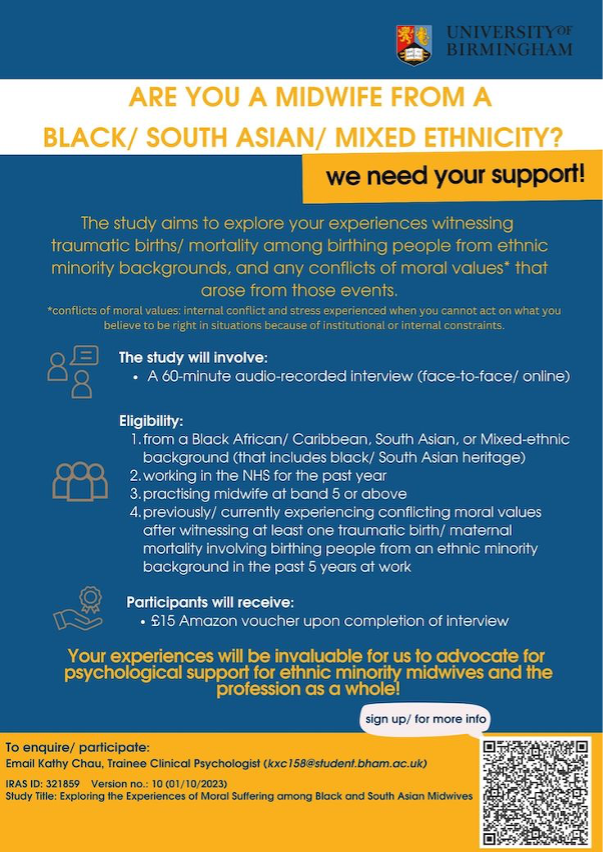
The health inequalities in people receiving maternity services have received growing concern in the country, where pregnant people from Black and South Asian backgrounds were reported to face double to triple the risks of dying during pregnancy [1], and systemic racism has been suggested to contribute to the issue [2]. I am a final year student of the Doctorate in Clinical Psychology programme at the University of Birmingham, and my research project is to explore the moral suffering (including moral distress and moral injury) among midwives from Black and South Asian backgrounds.
Previous research studies around health inequalities were mainly on pregnant people’s experiences, but not from midwives’ perspectives. This is the first-ever research study to explore the experiences and impacts on minority ethnic midwives at the personal, social, and professional levels of life. We hope the project will facilitate our understanding of minority ethnic midwives’ psychological needs at work, which paves the way for psychological support or systemic changes in the future.
In healthcare settings, moral suffering is defined by moral conflicts over whether the services provided are up to standard. It involves experiencing a moral event, psychological distress, and a direct causal relation between the two [3].
We understand from psychology that people experienced more vicarious empathic responses towards in-groups than out-groups in terms of ethnicity [4-6]. With the dual identity of being maternity staff and identifying as an ethnic minority, it is not uncommon for minority ethnic midwives to feel distressed and guilty after witnessing traumatic births or maternal mortality among women also from ethnic minorities, even when they have followed National Health Service (NHS) standards and guidelines. If you have had these experiences and are eligible, please contact me (my email address is at the bottom of the article).
Eligibility:
(1) identify yourself from a Black African/ Caribbean, South Asian, or Mixed background (that includes black/ South Asian heritage) in the UK;
(2) have been working in the NHS England at least for the past year;
(3) practising midwives at band 5 or above;
(4) have witnessed at least one traumatic birth/ maternal mortality involving birthing people from black/ South Asian backgrounds in the past five years; and
(5) have the ability to give Informed Consent.
If you would like to participate in the study (a 60-minute remote interview), please email me (Kathy Chau), at kxc158@student.bham.ac.uk (lead researcher).
The deadline for recruitment will be on 30th April 2024.
[1] MBRACE-UK. (2024). Maternal mortality 2020-2022 [Data set]. https://www.npeu.ox.ac.uk/mbrrace-uk/data-brief/maternal-mortality-2020-2022
[2] Knight, M., Bunch, K., Vousden, N., Banerjee, A., Cox, P., Cross-Sudworth, F., Dhanjal, M. K., Douglas, J., Girling, J., Kenyon, S., Kotnis, R., Patel, R., Shakespeare, J., Tuffnell, D., Wilkinson, M., & Kurinczuk, J. J. (2022). A national cohort study and confidential enquiry to investigate ethnic disparities in maternal mortality. eClinicalMedicine, 43. https://doi.org/10.1016/j.eclinm.2021.101237
[3] Morley, G., Ives, J., Bradbury-Jones, C., & Irvine, F. (2019). What is ‘moral distress’? A narrative synthesis of the literature. Nursing Ethics, 26(3), 646-662.
[4] Cheon, B. K., Im, D.-m., Harada, T., Kim, J.-S., Mathur, V. A., Scimeca, J. M., Parrish, T. B., Park, H. W., & Chiao, J. Y. (2011). Cultural influences on neural basis of intergroup empathy. NeuroImage, 57(2), 642-650. https://doi.org/https://doi.org/10.1016/j.neuroimage.2011.04.031
[5] Eres, R., & Molenberghs, P. (2013). The influence of group membership on the neural correlates involved in empathy. Frontiers in human neuroscience, 7, 176.
[6] Gutsell, J. N., & Inzlicht, M. (2011). Intergroup differences in the sharing of emotive states: neural evidence of an empathy gap. Social Cognitive and Affective Neuroscience, 7(5), 596-603. https://doi.org/10.1093/scan/nsr035


