Postnatal care is an important aspect of midwives’ roles in the UK and other countries. It is also important for women and families, yet it is known that it is a challenge to meet needs appropriately, especially in the current climate of staffing. Elizabeth Duff, until recently Senior Policy Advisor for the NCT, shares her concerns about the lack of action on postnatal care and encourages us to use International Women’s day as a platform for change
_________________________________________________
Ten years ago, Professor Dame Sally Davies, then Chief Medical Officer for England, published her 2014 annual report ‘The Health of the 51%: Women’, which included the stark statement that:
‘current postnatal care is not fit for purpose, lacking any basis in either evidence or maternal needs’ [1].
The consequences of this inadequate care in terms of maternal deaths are shown in an infographic:
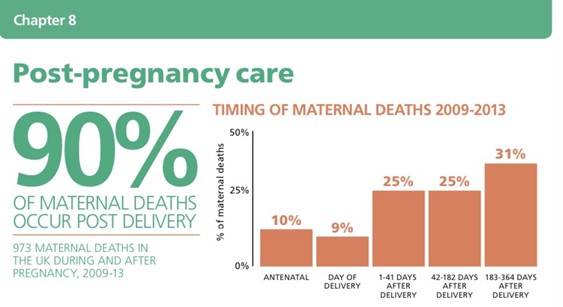
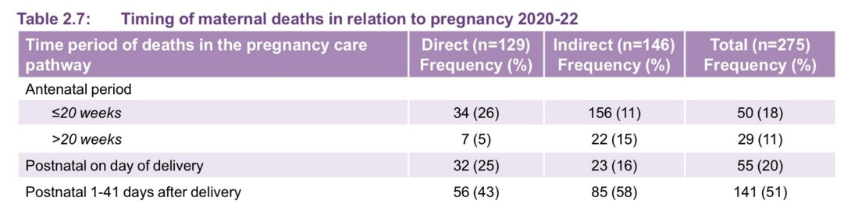
These data were taken from the contemporary MBRRACE-UK maternal mortality research. While there is no directly comparable graphic in the latest report, the table showing timing of maternal deaths confirms a large majority of the women who died were in the postnatal period birth to six weeks; and the text adds that late maternal deaths (six weeks to one year) continue to rise: in the triennium 2020-22, there was a mortality rate of 16.22 per 100,000 maternities compared to a late pregnancy-related mortality rate of 13.66 per 100,000 in 2009-11[2].
This chapter further confirmed that:
‘Postnatal contacts offer opportunities to identify and implement effective care to reduce maternal morbidity and promote longer-term physical and mental health, including improved outcomes of subsequent pregnancies and family health. Current service provision and content is not utilising these opportunities’.
These words, – both the summarised benefits of postnatal care and the missed opportunity of failure to provide it, – remain absolutely true today.
Writing now, available reports of women’s experiences of postnatal care suggest that the quality of this service has substantially worsened over years of staffing shortage as well as the devastating – and lasting – impact of the Covid-19 pandemic [3] [4].
This week brings International Women’s Day (IWD) 2025 with its driving theme ‘Accelerate Action’ [5]. Given that, in the UK, the Chief Medical Officer had urged prompt action on postnatal care 10 years ago, I hope we can be stimulated again to mark IWD with vigorous efforts to update care for women that will, in Dame Sally’s words ‘promote longer-term physical and mental health, including improved outcomes of subsequent pregnancies and family health’.
Since 2015, I have been personally involved in efforts to raise awareness of the desperate need for improved care for mothers at every stage:
- The ‘Hidden Half’ campaign run by NCT successfully demanded that the six-week postnatal check for mothers in primary care should be fully funded and mandated in the GP contract in England [6]
- A postnatal symposium ‘Better Births but worse postnatal care?’ was convened in 2019 when Professor Debra Bick and Dr Judy Shakespeare (both significant contributors to the CMO report cited above) joined NCT to bring together leaders from RCM, RCOG, iHV and relevant charities to focus on the topic [7]
- Professor Helen Cheyne and I presented a poster at the International Normal Labour and Birth Research Conference 2022 headed ‘I didn’t know what was normal!’ – a phrase often heard from new mothers experiencing worrying symptoms after the birth [8]
- In February this year, I attended a summit conference in Amsterdam, the Netherlands, organised by the international Postnatal Support Network and with an agenda based upon a global review of postnatal care [9]. I reported on this initiative at the London Maternity & Midwifery Festival 2025.
I also gave a talk to the Maternity & Midwifery Forum in 2022 on ‘Blood, sweat and tears: mothers’ body fluids & patriarchal distaste for postnatal care’ (Elizabeth Duff – Postnatal Care – Who Cares? #MidwiferyHour) This picks up the theme of mothers’ not knowing whether their loss of bodily fluids is a ‘normal’ consequence of the birth or a marker of serious haemorrhage, pyrexia, depression. Incidence of pus in a surgical scar, unexpected vomiting and uncontrolled loss of urine are also all worrying symptoms that may need urgent care but can be difficult for women to disclose without privacy and trust in a caregiver.
In spite of all these efforts and the endeavours of many others, postnatal care remains a dangerously threadbare service: fragmented between acute care, community midwifery, health visiting and primary care; challenging – sometimes impossible – to navigate for new parents.
The NHS in England is proposing major shifts in its overall approach, including: acute care to community care; and treatment of sickness to prevention. The new contract with GPs also has an emphasis on the benefits of continuity of care. I believe these three themes are integral to postnatal care and anyone responding to the NHS’s consultations, nationally or locally, should identify this service as a focus for urgent change:
- Community care is where the vast majority of postnatal care should take place, first in the family’s home then at a local, accessible and familiar health hub, where not only can parents meet and talk to each other but crucially professionals – midwives, HVs, GPs – may do the same
- Prevention of sickness is a significant role of postnatal care. Identification of deteriorating wellbeing in a mother, along with advice and reassurance about the legacy of pregnancy complications, can reduce the risk of serious harm in later pregnancies and later life. It may mitigate the current devastating incidence of suicides in the late postnatal months.
- Continuity of care is also vital. While it may not be possible to have the same individual caregiver, co-ordination of care can play a huge part. Maternal deaths happen when women ‘fall through the gaps’ in our present, hopelessly fragmented system. Integrated care boards (ICBs) can commission a service that works for women, works for professionals and turns back the frightening tide of postnatal maternal mortality.
Please accelerate your action: push these arguments; remember that functioning postnatal care will be not part of the problem, but part of the solution.
References
- Bick D, et al. Post-pregnancy care: missed opportunities during the reproductive years. Chapter 8 in Davies, S.C. “Annual Report of the Chief Medical Officer, 2014, The Health of the 51%: Women” London: Department of Health (2015) https://assets.publishing.service.gov.uk/media/5a80cc0ae5274a2e8ab52380/CMO_annual_report_2014.pdf
- Felker A, Patel R, Kotnis R, Kenyon S, Knight M (Eds.) on behalf of MBRRACE-UK. Saving Lives, Improving Mothers’ Care Compiled Report – Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2020-22. Oxford: National Perinatal Epidemiology Unit, University of Oxford 2024. https://www.npeu.ox.ac.uk/assets/downloads/mbrrace-uk/reports/maternal-report-2024/MBRRACE-UK%20Maternal%20MAIN%20Report%202024%20V2.0%20ONLINE.pdf
- Care Quality Commission. Maternity Survey 2024. https://www.cqc.org.uk/publications/surveys/maternity-survey
- Holly, J. Women’s experiences of maternity care. NCT, 2022.
- International Women’s Day 2025 ‘Accelerate Action’. https://www.internationalwomensday.com/Theme
- NCT Let’s get postnatal mental illness out of hiding. NCT, 2020. https://www.nct.org.uk/get-involved/campaigns/hidden-half-campaign
- Duff E, Bick D, Shakespeare J. Better Births but worse postnatal care? Designing a service fit for 2020 and beyond. NCT, 2020.
- The 21st International Normal Labour and Birth Research conference. Aarhus, Denmark, 2022. https://www.qmnc.org/international-normal-labour-and-birth-conference-2022/
- Herschderfer K, Cupelin E, Bal I. Postnatal rEvolution recommitting to care and support during the fourth trimester. Postnatal Support Network, 2024. https://postnatalsupportnetwork.com/
Elizabeth Duff, previous Senior Policy Advisor for the NCT
March 2025


