Climate change is a major concern globally, and healthcare has responsibility to address how to provide care and services that is more sustainable. Angela Willis, Hazel Ward Manager and Chief Sustainability Officer clinical fellow alumni 23/24 at GWH, Swindon, shares how their Trust have started to address sustainability and encourages us to examine our practises.
_____________________________________________________
Note this article will refer to women throughout, but it also includes birthing people
Climate change and the physiological impacts on pregnancy
Climate change caused by increasing global temperatures and carbon emissions has health consequences for humans. Climate change increases the incidences of wildfires, flooding, heatwaves, vector borne illnesses, air pollution and other adverse weather events. Women, children and the elderly are more vulnerable to the impacts of climate change due to the physiology1. There are many impacts of the effects of climate change on fertility and pregnancy. Exposure to either ambient air pollution or air pollution caused by wildfires due to extreme heatwaves increases the chance of pre eclampsia, IUGR, pre term birth and increases the chance of asthma in children1,2,3. Exposure to extreme heatwaves has correlational increases with stillbirths (greatest chance amongst Black and Hispanic women, highlighting the impacts on the most deprived communities), pre term birth, developing gestational diabetes, placental abruption and chorioamnionitis. Environmentally, air pollution and the extreme weather events caused by climate change also have impacts on the cardiovascular system which due to the physiological changes occurring during pregnancy increase the susceptibility to adverse health effects in pregnant women1,2,3.
The carbon emissions of healthcare and contribution to climate change
Healthcare globally is the fifth biggest industry sector of carbon emissions. In the UK carbon emissions from the NHS account for 4.7% of all UK emissions, is the biggest public sector contributor of carbon emissions and is just behind the aviation sector contributing 5.4% towards UK emissions. 1 in 20 cars on UK roads every day are for the NHS, whether that is staff, patients or visitors of NHS services. Whilst the healthcare sector will be impacted more as the effects of climate change increases, the carbon emissions released by healthcare is contributing significantly to climate change4. As a result, the Health and Social Care act in 2022 mandated in law for the NHS to reach net zero for all direct emissions by 2040 (things we can directly control or influence, like our buildings, energy generation, anaesthetic gas usage) and to reach net zero by 2045 for everything the NHS does not have direct control over (supply chain of medicines and equipment for example). The NHS already places a 10% social value weighting on procurements, and the implementation of the Evergreen assessment this year is placing more emphasis on suppliers to the NHS to address their carbon emissions towards net zero5.
The table below shows the average carbon emissions created by each contact or activity point with service users to highlight the hotspots of clinical care. The UK Healthcare Alliance on Climate Change has five key priorities to tackle the carbon emissions of care systems and organisations, and priority five highlights the need to change and transform health and care services6.
Average carbon emissions (KGCO2e) by NHS activity
| Activity | Kg CO2e | Local Substitution (KgCO2e) |
| In-patient bed day (low intensity/general | 37.9 | |
| In Patient bed day (high intensity/ICU) | 89.5 | |
| Outpatient midwifery or obstetric video consultation | 0.06 | |
| Home visit (travel to/from acute site) | 5.3 | *Local mileage |
| Staff travel to/from GP surgery | 1.26 | *Local mileage |
| Patient travel to/from hospital | 4.4 | *Local mileage |
| Patient travel to/from community hospital (Freestanding maternity unit) | 3.35 | *Local mileage |
| Emergency department visit | 13.8 | |
| Ambulance journey to hospital | 56 | |
| Outpatient (acute unit) attendance | 22 | |
| Midwifery appointment in a GP setting | 9.9 | |
| Homeworking (office equipment) | 0.032 per FTE working hour | |
| Homeworking (heating) | 0.31 per FTE working hour | |
| Home energy | 7.4 per 24hr |
Table: Clinical activity carbon emissions factors for care pathway appraisal V0.1 April 20247
Triple bottom line
The triple bottom line is a framework which highlights the benefit of focusing and tackling sustainability8. Often, when addressing environmental sustainability there are other benefits for the health and wellbeing of populations, such as improved finances for organisations or integrated care systems alongside increasing the value of health and social care. Quality Improvement in healthcare is one way to drive improvements in healthcare and can be combined with a framework called ‘Sustainable quality improvement (SUS QI).’ The SUS QI framework developed by the Centre for Sustainable healthcare focuses on the triple bottom line when improving environmental sustainability in healthcare.
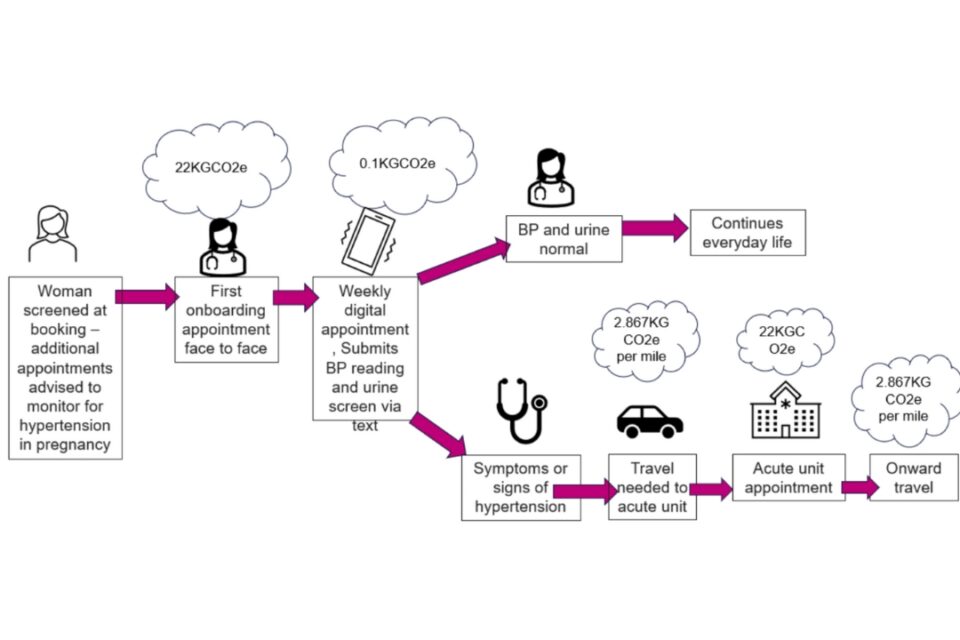
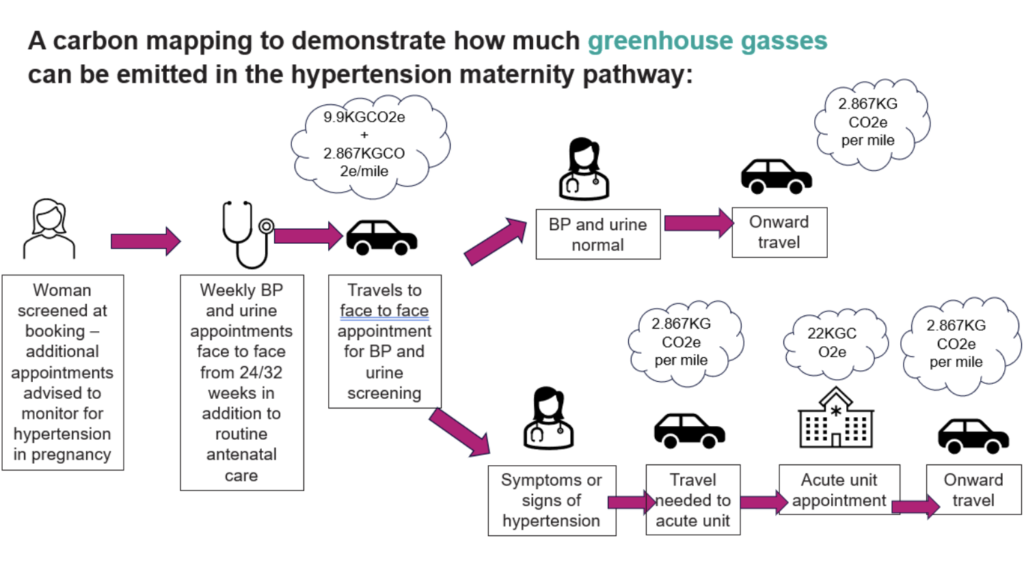
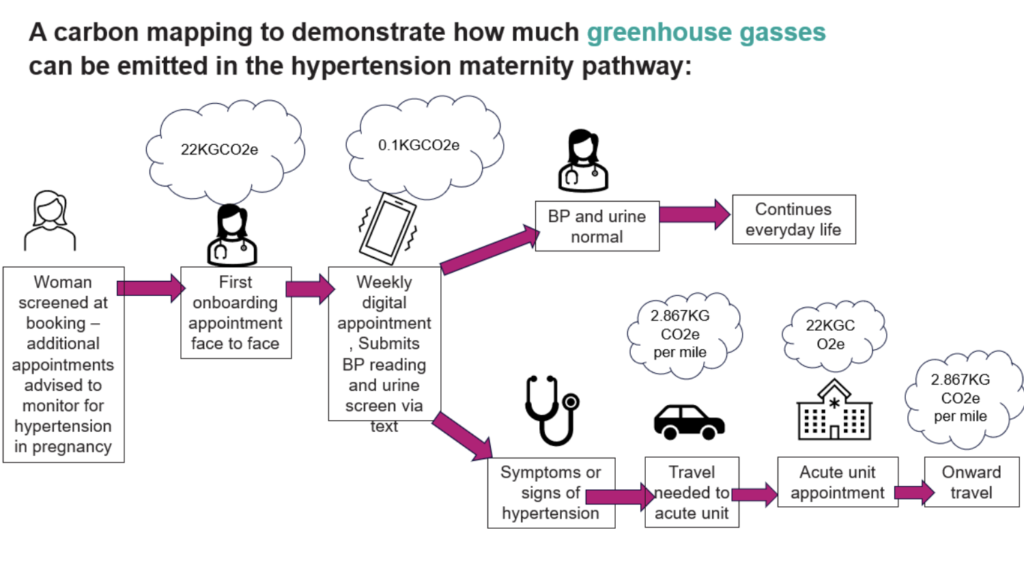
Sus QI in Healthcare begins with studying the current care pathway. Carbon emissions can then be applied and multiplied by the number of appointments/visits or people using the service. Through this method, carbon ‘hotspots’ are found and the care pathway or system appraised to look at how reductions in carbon can occur through lower carbon models of care. In collaboration with feedback from service users and staff, it identifies new and different ways of working with the intention of providing better value based healthcare for patients and staff. The care pathway for women at the greatest risk of developing hypertension in pregnancy is provided as an example below, where the care pathway is mapped out and the hotspots in the pathway can be seen, alongside the elements of the pathway which provide the greatest value and benefits for women and staff, and alternative ways to provide the care needed.
Hypertension in pregnancy pathway
Hypertensive diseases affect 8-10% of all pregnant women in the UK. The MBRRACE report highlights pre-eclampsia still accounts for 4% of all maternal deaths in the UK9,10. In addition the rate of women entering pregnancy with chronic hypertension is increasing and this effects 0.6-2.7% of all pregnancies here in the UK9. Neonatal mortality and morbidity increases with maternal hypertensive disorders which increases the chance of preterm birth and future health inequalities. Hypertensive diseases are proliferating with increasing maternal age, pre-existing medical comorbidities and rising obesity rates across the Western world.
Hypertensive diseases during pregnancy are also more prevalent amongst the most deprived populations and communities, living in areas of high air pollution, in women who are obese and in women who are of black or global majority ethnicity. Screening for hypertension in pregnancy enables prompt treatment and intervention such as growth scans, fetal monitoring and surveillance with timely birth to reduce maternal and neonatal morbidity. In many cases, early screening and treatment can help stabilise maternal blood pressure and continue the pregnancy towards term where the complications of preterm birth decrease.
NICE guidelines (2019) recommend women at the greatest risk of developing hypertension during pregnancy should be offered aspirin from booking to reduce the chance of developing pre-eclampsia. For women who develop gestational hypertension additional appointments to screen for proteinuria, raised blood pressure and symptoms of hypertensive disease should be undertaken in addition to weekly fetal monitoring and growth scans. These additional appointments increase the carbon emissions of the pathway, particularly if offered face to face. These additional appointments also add further pressure on maternity services and staff to provide the additional care, and require women to take time off work, to travel to appointments and, if they have other children, to find childcare provision to attend appointments.
‘Go Flo’
In 2017, the increased demand to provide additional appointments for women either with diagnosed gestational hypertension, or for women at the highest risk of developing hypertension led to a collaboration between the Maternity team at the Great Western Hospital (GWH) and Health Innovation West to implement the ‘Go Flo’ service. The Go Flo service enables women to monitor their blood pressure at home by providing education and blood pressure monitors. Women share their results via a text messaging service, which reduces the need for unnecessary appointments.
| Reasons for offering Home Blood pressure monitoring service in pregnancy |
|
The Swindon service is led by a ‘Go Flo’ Midwife, providing ‘onboarding’ appointments to women who have been referred and consented to be part of the service. During the appointment, women are provided with education of ‘what is normal’, education on signs and symptoms of hypertensive disorder to be aware of and how to use the blood pressure machines, text messaging service and dip their urine. The midwife checks each women’s results on a weekly basis. Blood pressure monitors are returned at the end of pregnancy ready to use again for future women enrolled into the service.
Operating the Go Flo service through the antenatal clinic requires 85 hours of clinician time to complete the onboarding appointments. It is difficult to quantify the exact hours needed to support the follow up of the women on the service as the text messaging service has automatic prompts to remind women to submit their urinalysis and blood pressure monitoring. However, the estimated time to follow up each patient is 30-60 minutes a week (on average) which equates to 85-170 clinician hours a year to run the service.
Care pathway and carbon Hotspot prior to ‘Go Flo’
Care pathway and carbon Hotspot following ‘Go Flo’
The Carbon Footprint of Go Flo at GWH
Six months of data was obtained of the Go Flo service from women on the pathway in May-October 2023. The carbon footprint was calculated using the distance between women’s postcodes, GP surgeries and the secondary care unit postcode (for women who were medicated), applying the NHS futures carbon footprinting data for average outpatient secondary care appointment (22KGCO2e) and appointment with a midwife in the primary care practice (9.9KGCO2e), alongside using the government emissions data for 2023 at 0.28676KGCO2e/mile (representing 58% of all UK car journeys). Urinalysis sticks and blood pressure monitors have not been taken into consideration within the carbon footprint as regardless of which service is provided, both would be used. In addition, routine antenatal care appointments were not included in either of the calculations. This audit looked purely at additional appointments provided.
Key Findings from the audit
- In total there were 896 appointments across 83 women in the six months of audit data.
- 85 women joined the pathway, 2 left the pathway due to moving geographical location in pregnancy
- 68 of the 896 appointments had abnormal observations or symptoms and needed to be seen face to face in the antenatal assessment unit
- 29 women required medication for hypertension during pregnancy (35%) and continued to be monitored through Go Flo once a week, and having one face to face appointment in the assessment unit a week
- A further 3 women (4%) of women were commenced on medication and had birth expediated for pre-eclampsia the same week as the positive screen for hypertension in pregnancy through Go Flo
| Total number of women on Home BP monitoring | Total number of women who
required medication |
Total number of women who had birth expediated same week | Total number of women who
continued with increased Home BP monitoring & DAU attendance |
Number of women who developed hypertension again & previously had hypertension |
| 83 | 32 | 3 | 29 | 11 |
| Total of number of appointments (twice weekly) needed (either in assessment unit or community midwife setting) | 376 | |||
| Total number of appointments through OHP | 118 | |||
| Total carbon reduced by using OHP vs FTFP for medicated hypertension in pregnancy | 3,147KGCO2e | |||
Key findings from the women who were medicated for hypertension in pregnancy
Carbon Footprint of the service in a year based on the six month audit data obtained
- Providing the additional appointments as a face to face appointment either in the GP surgery with a community midwife or in the antenatal assessment unit once medicated equates to 27,109KGCO2e each year – the equivalent of 5 premium economy flights London-Hong Kong return and driving once London to Glasgow return.14
- Providing the additional appointments virtually through Go Flo has a carbon footprint of 4,846KGCO2e – the equivalent of 1 return flight London to Hong Kong return premium economy, and one flight Heathrow to Glasgow return.14
- The home blood pressure monitoring service saves 22,209KGCO2e a year.
- If this service was rolled out nationally it has the potential to save 3.34 millionKGCO2e annually based on average of 25,000 women identified as high risk at the booking in appointment of developing hypertension in pregnancy on 2022 birth statistics – the equivalent of flying premium economy London-Hong Kong 742 times.14 This figure could be higher for women without risk factors who develop hypertension without pre-eclampsia and require additional appointments once diagnosed.
The triple bottom line benefits of Go Flo
Whilst the scope of this article concerns hypertension in pregnancy, it does raise the question of how many other care pathways could be delivered in a similar way? Consider VBAC (vaginal birth after caesarean) as an example, is there an opportunity to provide a group consultation either in person or digitally with a midwife at 20 weeks to provide the general information and signpost people to one to one debrief if needed? This could provide social benefits to other women, reducing obstetric appointment pressures and lower waiting lists, whilst also reducing the carbon footprint of the pathway. An individual call with an obstetrician or consultant midwife for the decision can occur around 36-38 weeks with only 1 face to face appointment outside of the routine midwifery appointments if a caesarean is chosen. That one stop appointment will include the anaesthetic appointment, pre op bloods, swabs a few days before the appointment, meaning less travel and transport for the woman.
Another example is childhood asthma, where providing group consultations could provide social benefits for parents, whilst providing one session where all the information is given and a ten minute individual consultation. This could increase appointment capacity, reducing primary care pressures.
Every midwife has the ability to make a difference. Every midwife has the ability to make a change whether in their professional or personal life. One small footprint all working collectively together can improve the planet’s health and in turn the children of tomorrow and women of today’s health too.
Acknowledgements: A huge thank you to Nusrat Fazal and Anne Webb for setting up the service in 2017, to all the GWH assessment unit staff and to Becky Tollafield for all the help on auditing, understanding the pathway and for being the current lead for the service.
Reference list
- Segal, Giudice Systematic review of climate change effects on reproductive health. 2022 Fertility and sterility 118(2) Available from: Systematic review of climate change effects on reproductive health – PubMed (nih.gov)
- Mitku et al. Impact of ambient air pollution exposure during pregnancy on adverse birth outcomes: generalized structural equation modelling approach | BMC Public Health | 2023. https://bmcpublichealth.biomedcentral.com/counter/pdf/10.1186/s12889-022-14971-3.pdf
- Chief medical officer. Chief medical Officer’s Annual report 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1124738/chief-medical-officers-annual-report-air-pollution-dec-2022.pdf
- NHS England. Delivering a ‘Net Zero’ National Health service 2022. B1728-delivering-a-net-zero-nhs-july-2022.pdf (england.nhs.uk)
- NHS England Evergreen Sustainable Supplier Assessment. 2024. NHS England » Evergreen Sustainable Supplier Assessment
- UK Health Alliance on Climate change UK Health Alliance on Climate Change
- NHS England. Clinical activity carbon emissions factors for care pathway appraisal V0.1 April 2024 Future NHS platform Clinical activity carbon emissions factors for care pathway appraisal.
- Elkington, J. Enter the Triple Bottom line 1994. 1-15 https://johnelkington.com/archive/TBL-elkington-chapter.pdf Accessed August 21 2024.
- NICE. Hypertension in pregnancy: How common is it? Chronic hypertension reference https://cks.nice.org.uk/topics/hypertension-in-pregnancy/background-information/prevalence/#:~:text=Prescribing%20information-,How%20common%20is%20it%3F,rates%20of%204.2%E2%80%937.9%25. May 2022.
- Knight et al. Saving Lives, Improving mother’s care. Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into maternal Deaths and Morbidity 2019-2021. 2023. Available from: MBRRACE-UK_Maternal_Compiled_Report_2023.pdf (ox.ac.uk)
- Fazal et al. Telehealth: improving maternity services by modern technology. BMJ Open Qual 9(4). 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7640525/
- Fazal et al. Empowering pregnant women to “go with flo” and monitor their blood pressure at home using telehealth technology 2020 Go Flo poster v.07 CJB 08.05.2018.pdf (Florence. Community)
- Paterson et al. (2023) Qualitative Evaluation of a rapid rollout of home blood pressure monitoring during Covid-19. 2023. PLoS ONE. 18(3) https://www.pure.ed.ac.uk/ws/portalfiles/portal/340886044/journal.pone.0278156.pdf
- Berners-Lee M. How bad are Bananas: The carbon footprint of everything. Pg 140 Flying London to Hong Kong. 2020.Profile Books Ltd: London.
Angela Willis
Ward Manager GWH, Chief Sustainability Officer clinical fellow alumni 23/24 angela.willis5@nhs.net
September 2024