In October 2024 a significant independent report that examined how to enable safe quality maternity care in Northern Ireland was released. It reported on widespread concerns about the service, and importantly, provides a blueprint for improvements and change, which may be replicated across other countries. We are privileged Mary J Renfrew OBE LLD FMedSci FRSE, Professor Emerita, University of Dundee, author of the report, shares a summary and indicates the way forward.
_________________________________________________
Background
In May 2023 I was commissioned to conduct an Independent Report in response to concerns about the safety of midwifery care in Northern Ireland (NI)- a Coroner’s report following the death of a baby raised specific concerns about care in freestanding midwifery-led units, and there were wider concerns about the safety of midwifery services. The report was published in October 2024 and has been positively received by the government of Northern Ireland, which has committed to implementing the recommendations. It is the first report on maternity services in the UK to examine a whole health system, drawing on an evidence-informed analysis to identify transformative solutions. The full report, and a summary, can be found at this link . The government response is here . In this blog, I will summarise the report and draw out some lessons for other countries to consider.
Aim of the report
There were three detailed terms of reference; two directly requested by the Coroner that related specifically to freestanding midwifery-led units, and one to examine the wider midwifery and maternity services. The overarching aim was:
to identify the key conditions for safe, quality midwifery services in all settings in Northern Ireland: evidence-informed, equitable, safe, respectful, and compassionate midwifery care should be available for all women and newborn infants wherever and whenever care takes place.
Context
To understand the factors affecting women, babies, and families and the maternity services, it is essential to know the social and health context. In Northern Ireland some key factors include:
- NI has the highest proportion of the population living in most deprived quintile in UK
- There is a population of around 1.9 million, and approximately 20,200 babies are born annually; almost all in hospitals across five Health and Social Care Trusts
- There are five small alongside midwifery units; all freestanding midwifery units were closed at the time of this work
- NI had the highest rates of stillbirths, perinatal and neonatal deaths in the UK at the time of this report – stillbirth rates decreased slightly in the most recent MBRRACE report (MBRRACE 2024)
- Induction of labour and caesarean birth rates are higher than they have ever been; 38% and 40% respectively, and still rising; while similar to other UK countries and to the Republic of Ireland, these rates are out of step with similar countries internationally
- The complexity of maternity service provision is affected by increasing rates of poverty, maternal age, and rates of health conditions especially diabetes and obesity
- There is a legacy of political instability with ongoing adverse impact on funding of public services
- There are longstanding workforce shortages, especially of midwives
- There has been no maternity strategy in place since 2018
What we did and why we did it
We developed a novel methodology for this review to make sure we examined all the perspectives that matter in understanding all the factors that matter. Our structured methodology was developed in consultation with service user advocates and experienced researchers and practitioners. We started by identifying key principles to inform the work. We agreed that the work would:
- Have a core focus on the needs and views of all women, babies and families – human rights and equity were critically important perspectives
- Draw on high quality research evidence and data
- Be informed by meaningful collaboration and participation and widespread engagement with women and families, service user advocates, interdisciplinary staff and students, managers and policy makers
- Conduct an analysis of what works, using a strengths-based approach
- Consider interdisciplinary working in an enabling environment for all staff and students
- Take a whole system perspective to include practice, policy, workforce, education, research, leadership, culture, governance, and regulation
- Consider safety in all its dimensions – physical, psychological, social and cultural.
A series of interconnected steps included:
- in-depth engagement with women, partners, advocacy and community groups; and with interdisciplinary staff, students and educators, senior managers and policy makers
- comprehensive analysis of: data on outcomes, experience, workforce; eight rapid efficient reviews of key topics were conducted to identify good quality evidence; scrutiny of relevant policy; and information requested from Health and Social Care Boards and key organisations
- identification of fifteen positive service developments in NI and other countries
- a structured analysis of all the findings to inform feasible, sustainable, evidence-informed system-wide recommendations
- an Expert Group of UK and international researchers, practitioners, educators and service use advocates and an Advisory Group of NI colleagues and service user advocates ensured regional and national expertise at every stage of the process.
Importantly, we wanted to hear from women and partners with a wide spectrum of experience, across all socio-economic backgrounds and with positive as well as negative experiences. We worked to avoid re-traumatising women and their families at any stage, whether in recruitment or while we listened to them, and we ensured that they could access support after our discussion if they needed. The ways in which we did this are fully described in the main report.
It was important to analyse our complex set of findings in the light of good quality evidence on what a safe, quality maternity system should provide. To do this systematically, effectively, and accurately our analysis was structured around a set of key questions. The first set of questions was about care and services and was derived from the evidence-informed framework for Quality Maternal and Newborn Care from The Lancet (Renfrew et al 2014) which identified the components of care that all women and babies need. The second set of questions was about how the whole health system should work – including components such as governance, accountability, workforce, funding, and education – and was derived from a rapid efficient literature review conducted for this report by Mattison et al (2024); the full review is included in the main report.
What we found
Negative experiences
Many women and staff described serious deficits in care across the maternity journey, resulting in trauma and distress for some women, with physical and psychological damage for some women and babies. Many women described fragmented services where they had to tell their story over and over to different staff, which was especially difficult for those with previous negative experiences. Three key deficits in care were identified: a lack of support, information, and relationship-based care in pregnancy; a mismatch between current high induction levels and available beds and staff to care for women at this vulnerable stage; and women not receiving the postnatal care they need either in hospital or at home, especially following caesarean or traumatic births. Each of these deficits is resulting in compromised physical and psychological safety for women and babies, with constraints on women’s ability to make informed decisions and to give consent. Women’s negative experiences following birth affecting their physical and psychological health and their interaction with their babies were so widespread that postnatal care became the top priority for immediate action. Staff reported working in circumstances where they were stressed on a daily basis, with many describing an over-riding task focus, a lack of personalised care, a culture of fear in the labour ward, and at times, ineffective responses to escalation and adverse incidents. Psychological safety for staff was compromised, and was another key priority for action. Senior levels of the organisation seemed to be unaware of the extent of the problems being experienced by women and by staff.
When examining the factors underlying these findings, our analysis showed that:
- Northern Ireland does not have all necessary structures and processes to drive equitable, system-wide change
- There is a lack of integration and whole-system working across every setting – home, community, and all areas of hospital maternal and newborn care
- There are limited mechanisms for women’s and staff voices to be heard
- There are resource pressures for all, but they are especially challenging for midwives
- There is inconsistent and fragmented service delivery, silo working, and unclear accountability
- The current model of care, with very high intervention rates in labour and birth, has developed piecemeal without evaluation of effectiveness, and it is not matched by appropriate staffing
- Midwives were not able to practice their full scope of professional practice; the current model of care combined with resource pressures resulted in them being unable to provide the support and preventive care that women need throughout their maternity journey
- There is a task and process focus instead of a focus on the needs and preferences of women and babies, especially in labour ward
- Safety work is focussed on birth, hospital, and interventions – not on the whole maternity journey
- There is a lack of awareness of the key role of midwives especially in pregnancy and postnatally
- There is an over-riding culture of fear and blame, rather than an open learning culture
- A framework for effective interdisciplinary education and training is lacking despite its acknowledged importance
- There is limited scrutiny and evaluation especially of women’s experiences of care, mental and emotional health and wellbeing, and longer-term outcomes
- Staff wellbeing is not a priority despite problems of retention and high rates of sick leave
Positive experiences
At the same time, many women and partners reported a range of positive experiences. These included opportunities for information and respectful discussion, with evidence on outcomes and levels of risk; care that focused on prevention and support; kindness and compassion; reassurance, calmness, and a positive outlook; skilled, individualised care and respect for women’s views and decisions; relationship-based care; continuity of care and carer; and building trust in the staff caring for them. Women reported many staff doing their utmost to provide skilled and compassionate care while working in difficult circumstances.
Many staff members valued their experiences of positive service provision – they described staff acting as a resource for each other, supporting and working together to problem-solve; planned, respectful interdisciplinary team working to meet needs of women and babies, especially for women with complex clinical, psychological, and social additional needs; providing continuity of midwifery carer; effective leadership, communication, team working; and integrated and interdisciplinary education, training, and staff development.
Analysis of the fifteen examples of positive care and services showed that they shared characteristics including:
- Partnership working with women and families
- Positive interdisciplinary working at all levels of the system
- Shared focus, values, philosophy, vision, and culture
- Enabling and supporting midwifery care and services
- Ensuring evidence-based care and standards
Transforming maternity and newborn services
Our analysis has shown that individual actions to improve the quality of care are not enough – there is an urgent need for transformative change at every level of the system.
Key conditions for a safe, quality maternal and newborn health system
Seven key conditions have been identified to ensure safe, quality care and services in any maternity and newborn health system (Figure 1).

Figure 1: A Quality Maternal and Newborn Health System: key conditions. From Renfrew MJ. Independent Report on Enabling Safe, Quality Midwifery Services and Care in Northern Ireland. 2024. Department of Health Northern Ireland.
Every component of these key conditions is essential. This includes whole-system support for universal, accountable, quality midwifery care for every woman, baby, and family across the whole continuum of care. Midwives are the only health professionals there at every stage of the maternity journey for every woman and every baby, and who have a key role in prevention and in public health aspects of care as well as managing complexities when they arise. If midwifery is weakened or not available at every stage of the maternity journey, the safety of women and babies is compromised. Critically important is the need for the whole system to have a core focus on the needs of women, babies, families, and communities, and to ensure their meaningful participation in the design, delivery, and monitoring of services.
Ensuring safe, quality care and services across the whole maternity journey and in every setting – home, community unit, and hospital, is essential (Figure 2). Women and staff were very clear about the essential characteristics of care at every stage – respect, kindness, trust, relationship, continuity, prevention, support, and evidence.
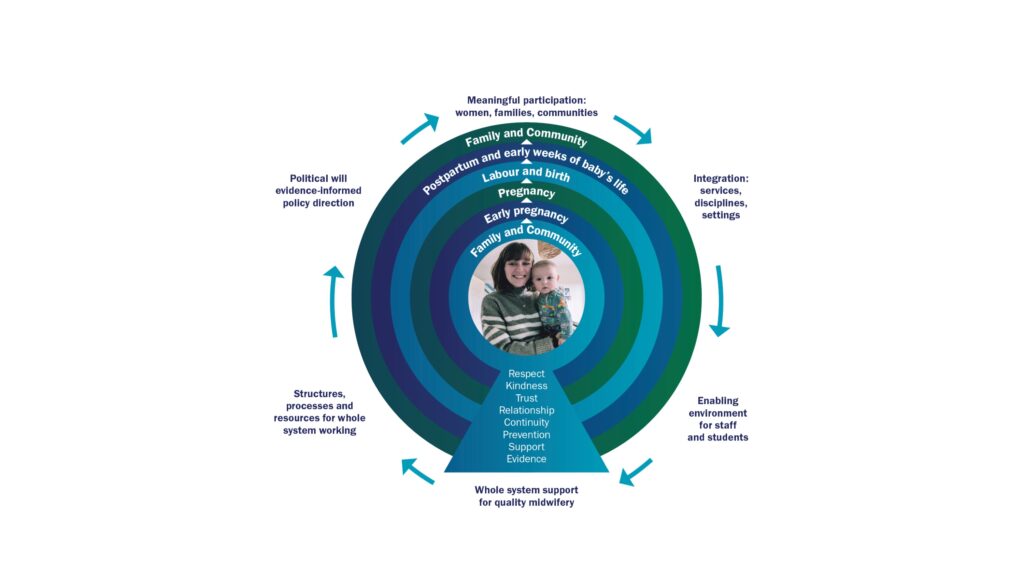
Figure 2: Key conditions for a quality maternal and newborn health system provided across the whole maternity journey. From Renfrew MJ. Independent Report on Enabling Safe, Quality Midwifery Services and Care in Northern Ireland. 2024. Department of Health Northern Ireland.
Action for system transformation
Three essential components emerged as essential (Figure 3).
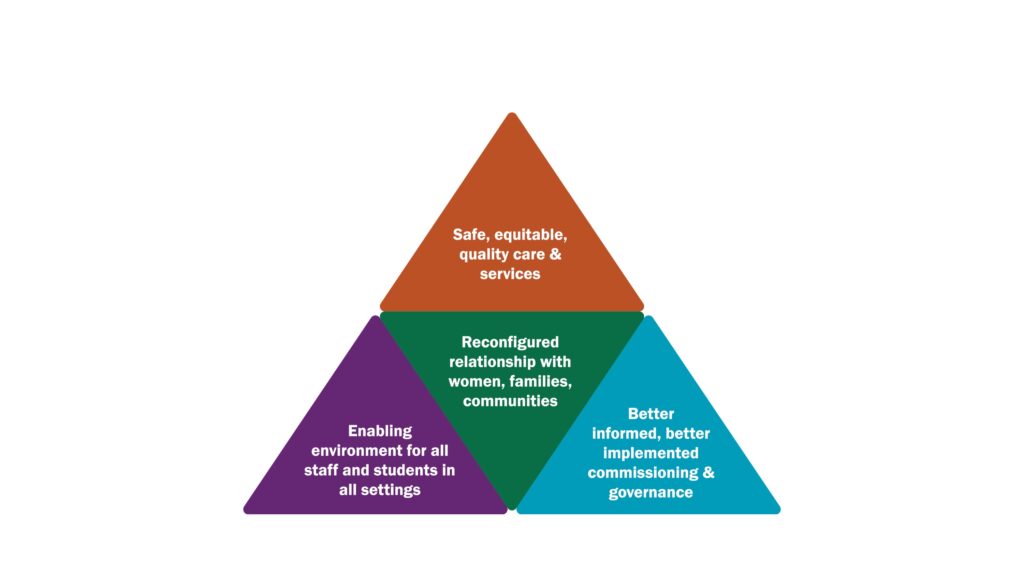
Figure 3: Three essential components to build safe, quality maternal and newborn care and services. From Renfrew MJ. Independent Report on Enabling Safe, Quality Midwifery Services and Care in Northern Ireland. 2024. Department of Health Northern Ireland.
Detailed recommendations were informed both by good quality evidence and by the views of our respondents. They include changes to introduce whole-region strategic developments to ensure consistent equitable care, to improve safe, quality care and services in all settings where care takes place, to improve systems for data, monitoring and review, to evaluate the current model of care, and to build capacity and capability for the future. All of these recommendations matter – in combination they build a safe maternal and newborn system. These are summarised in Figure 4.
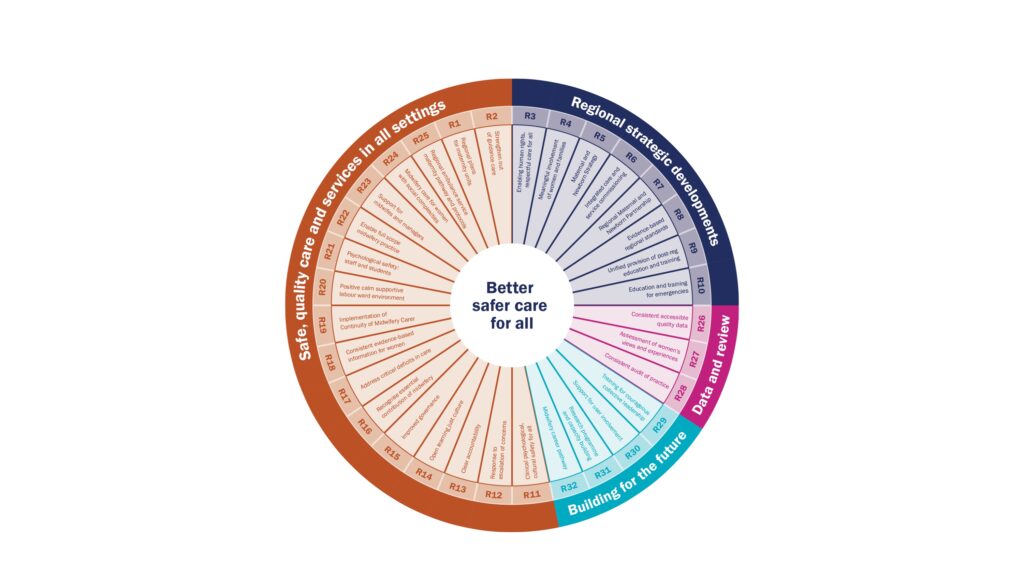
Figure 4: Summary of recommendations for transformative change. From Renfrew MJ. Independent Report on Enabling Safe, Quality Midwifery Services and Care in Northern Ireland. 2024. Department of Health Northern Ireland.
Why it matters
All women and babies must be safe – physically, psychologically, socially and culturally, in pregnancy, during labour and birth, and following birth. Not only does their safety directly affect their survival and immediate health and wellbeing, but physical, emotional, and mental health problems can persist and affect them and their families in the longer term. This work has shown that in Northern Ireland, outcomes and experiences for many women and babies are unacceptable, and out of alignment with current best evidence and international benchmarking. There is an urgent need to act.
What happens next
The report and its recommendations have been accepted by the NI government, and an implementation plan is being developed. Importantly, implementation work is being developed in collaboration with services user advocates, staff and managers at all levels of the system across Northern Ireland. While resources are limited, there are strengths to build on: women and families want to participate and be part of the solution; there are committed staff and students who want to work together to improve care; there are positive examples of successful services to draw on; and there is good quality evidence to inform the next steps.
What are the messages for the rest of the UK and beyond?
This work provided an opportunity to step back and reflect on what women, families, staff, and students were telling us about what is needed to ensure safe quality care and services for all, and to draw on good quality evidence to co-create evidence-informed, feasible, sustainable solutions. Much of what we learned can apply across other health systems. Some of the important lessons learned for all maternity and newborn care include:
- Identify and tackle underlying system-level factors
- Ensure the voices of women, communities, staff are built into all structures and processes
- Use a positive supportive approach, identify and celebrate success as well as address failure
- Ensure that shared values of respect, equity, trust, person-centredness, evidence-based information, and meeting community/population needs are evident in all governance and commissioning processes
- Consider physical, psychological, social, and cultural safety in all settings
- Use all relevant evidence and data to inform service planning, provision and monitoring
- Ensure and support provision of the full scope of midwifery care for all women and babies, across the whole continuum of care
- Ensure prevention, support, information, and relationship-based care as well as treatment
- Include the whole continuum of care and all settings in improving safety
- Provide practical support and leadership development for midwives at all levels
- Ensure senior midwifery representation in all governance and management forums
- The commissioning process must ensure an evidence-informed, cost-effective funding model
- Develop courageous, compassionate interdisciplinary leadership
- Provide education and support for all staff, managers, leaders
- Jointly tackle the culture of fear and blame, develop a pro-active open learning culture
- Build capacity and capability for the future – practice, education, research
A final word
How we care for women and babies is a measure of our society. In the course of this work, I had the privilege of encountering many people in Northern Ireland who share the understanding that pregnancy, birth, and the early weeks of life are fundamentally important for each woman, baby and family, and for communities and populations. There is a real appetite for change at most levels of the system. Positive change is possible – by working together to implement the recommendations it can be a reality.
Acknowledgements
This report would not have been possible without the input and support of many, many people. I am incredibly grateful to each and every one for giving their time and for providing key lessons for future services and care for women, babies and families. They were all truly instrumental in helping to shape the work and the solutions identified.
A full set of powerpoint slides of the report are freely available for use: https://www.health-ni.gov.uk/publications/enabling-safe-quality-midwifery-services-and-care-northern-ireland
References
MBRRACE-UK. Saving Lives, Improving Mothers’ Care, 2024. NPEU Oxford
Mattison CA, McNeill J, Lynn F, Renfrew MJ. Health system barriers and enablers to quality midwifery services. 2024. In: Renfrew MJ. Independent Report on Enabling Safe, Quality Midwifery Services and Care in Northern Ireland. 2024. Department of Health Northern Ireland.
Renfrew MJ. Independent Report on Enabling Safe, Quality Midwifery Services and Care in Northern Ireland. 2024. Department of Health Northern Ireland.
Renfrew MJ, McFadden AM, Bastos MH et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. 2014. The Lancet, 384: 1129-45
Mary J Renfrew OBE LLD FMedSci FRSE
Professor Emerita, University of Dundee
February 2025


