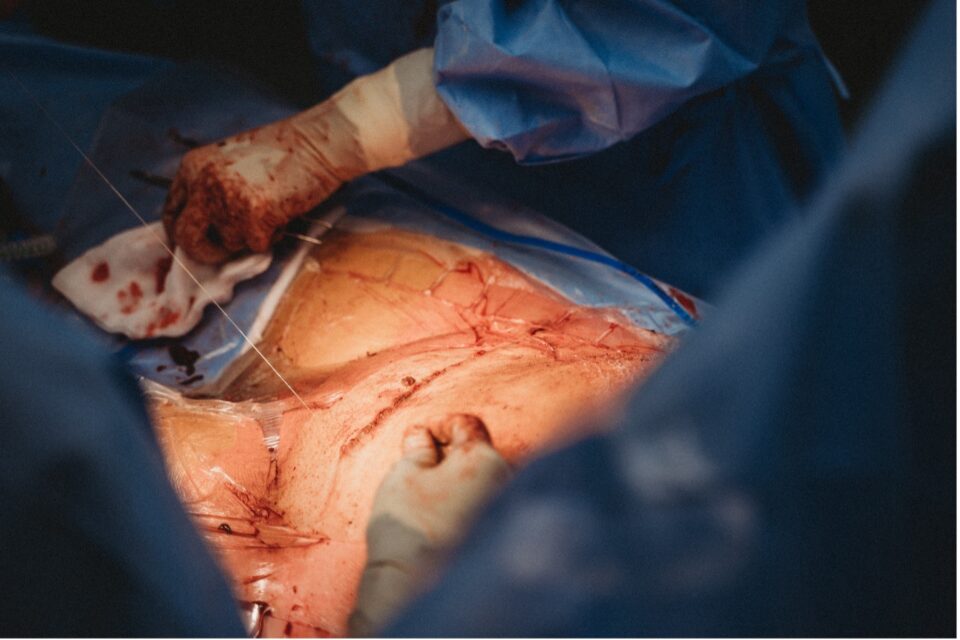
Globally the rates of Caesarean Section births are continuing to rise, with resulting impact on care required in the postnatal period. Janine McKnight-Cowan, Personalised Care Project Lead-Workforce Derbyshire Joined Up Care, explains the importance of ensuring appropriate care that will meet the needs of women and birthing people and support recovery.
______________________________________________________________________________________________________________________________________________________________________
April is ‘National C-Section Awareness Month’, and is the initiative of ‘The International caesarean awareness network who have been active since 1982. Their intention is to inform and educate the public about the reality of childbirth. One thing that is clearly transparent is that caesarean section rates in the UK are at their highest ever, over 30%.
This figure is constantly rising especially since the NHS no longer use C-Section rates as a means of measuring maternity unit performance. Since February 2022 maternity units were advised to follow NICE guidance and treat cases on an individual basis, rather than having to meet targets for C-Section births, following the first report into maternity services at Shrewsbury and Telford Hospital NHS Trust. The previous guidance was to promote vaginal birth and try to keep their C-Section rates at around 20%.
What does all this mean for maternity services, and why have a C-Section awareness Day?
For me, and my co-author of our newly published C-Section Recovery Manual, Your Body-Your Recovery. It is all about education, knowledge, and understanding; women need to know the choices they are making, the choices they can make and how we as health professionals support them to make informed, safe decisions about their birthing experience.
We have tools to support us to do this in clinical practice. We are now supported with new training materials to develop our skills in personalised care, (see box 1) and women in the UK should receive care that ensures, every woman and birthing person is entitled to personalised care. Tailoring this approach doesn’t just help deliver a better experience of care but contributes to their well-being and safety.
Course: Lived Experience Maternity Workforce videos (personalisedcareinstitute.org.uk)
So, if we are to keep up the conversation around c-section, including it as a birth choice, then should we as an NHS also be investing in the post-operative recovery from what is major abdominal surgery?
Sadly, we underestimate the recovery following c-section, perhaps as those who have not experienced it. In preparing for birth we lack a focus within antenatal education opportunity to fully educate women on the likelihood that birth could be by C-Section. On top of this, the transition from theatre either by choice or necessity, to investing in their holistic recovery at home, remains disjointed. Discharge is happening earlier, often within 24-48 hours; recovery information remains inconsistent, especially when it comes to wound care; coping strategies, pain management and transition to motherhood, is ignored, all following surgery.
How can we all help- which includes the family and friends support network at home?
Right now, we are seeing the ‘pause button’ in some places on continuity of care as the NHS maternity and health visiting services attempt to cope with a severe retention and recruitment problem. I mention health visitors as they are the service in the UK who provides continuity of care once a midwife discharges a mother to their care. In most cases this is around day 10 postpartum. For the C-Section mother, who has an abdominal wound, her healing is not over, her care needs to be transferred, her care plan should include wound management. Does it? Or in most cases, is the mother left to maintain her own wound?
These are very disturbing grey areas around post-partum C-Section recovery that need further clinical support.
Given that most c-section surgical site wounds can dehisce at around day 10-21 isn’t it vital the whole post-partum care team are alert, and aware of the possibility of wound complications like, wound separation, and surgical site infections (SSI)? Given that 3-15% of women will develop an infection in the post-partum period it is vital women know what to look for, who to tell, and how to prevent severe complications like wound dehiscence, and sepsis (Rastas & McKnight-Cowan, 2022).
Recommendations from NICE (2013) Statement 7 suggest people having surgery, including c-sections, are cared for by healthcare providers that monitor surgical site infection rates (including post-discharge infections) and provide feedback to relevant staff and stakeholders for continuous improvement through adjustment to clinical practice. NICE also recommend that wounds should be monitored for up to 30 days. (National Wound care Strategy 2021)
The World Union of Wound Healing Societies (WUWHS 2018) have numerous models for assessment of wounds; one of their summaries of SSI’s indicates some alarming statistics for mothers in their post-partum period. SSI as defined by the Centres for Disease Control, as an infection that presents up to thirty days after a surgical procedure and can appear at different times.
- 55% of SSI’s are detected within 10 days of caesarean section
- 75% of SSI’s are detected within 14 days
- 90% of SSI’s are detected within 20 days (WUWHS 2018)
Given these statistics, it is vital all women and all health professionals caring for them are aware of the risks associated with postpartum c-section wound recovery. Yet, mothers are discharged with a lack of continuity and consistency of care, disjointed clinical record keeping, without discharge records ideally recording ‘state of wound at discharge’. At the time of writing both the book and this article I have been unable to get hold of a validated discharge pathway for C-Section wound management that includes the interprofessional discharge from maternity services to health visiting services.
If our policy strap lines are shared care, personalised, and intended to be risk free, then we need to extend care guidelines into post-partum recovery following C-Section, that includes the risk to mothers of SSI’s and wound dehiscence.
Mothers need to be forewarned to be forearmed, and the simplicity of one of the tools within the new manual SCAR TRACKER@ does just this.
The challenges for C-Section post-partum women are numerous, not only wound care, and this can be most challenging. It includes pain management, basic coping mechanisms, transition to motherhood, breast feeding, maternal mental health, leaving hospital, adjusting to home, siblings care, daily home chores, diet, fatigue, sleeplessness, in some cases post traumatic triggers, anaemia, challenging medical conditions, and caring for a new-born. It is no wonder why, mothers who have an emergency C-Section are 15% more likely to experience post-natal depression (Tonei 2019).
The rhetoric is clearly there; the transporting of health promotional advice is neither consistent nor sustainable across the NHS. Mothers who have had a C-Section will, and clearly do turn to media platforms to gain advice and support, and there is an unbelievable social media movement on C-Sections across Facebook, Instagram, and Twitter. Some highlight disturbing wound pictures, and the advice that may be given is unregulated. Simply, mothers ‘need help@home’. How they get this help, support, and care is both complicated and costly. Discharge visits are now reduced, and in both maternity and health visiting services are stretched to capacity.
So, what can we celebrate this April 2023 ‘National C-Section Awareness Month’? A new C-Section Recovery Manual, a new maternity professional book, a labour of love, a legacy to a combined eighty-five years of maternity and community care of women. A manual that has twelve C-section chapters of information, a manual that has recovery tools, a SCAR TRACKER@ for wound management, daily planners for recovery management to be shared by mother’s support networks at home; coping mechanisms, a full index of medical explanations, industry top tips and much, much more. A manual for mothers, and their support networks, a manual for student midwives, and health visitors to adopt the personalised values and truly share with mothers ‘what matters’.
If we are unable be at home with them, then we can recommend healthcare @ home in the form of a well written and professionally written book, for new mothers who have or are going to birth by C-section. An evidence-based manual written with wit and wisdom, consistent, so mothers can record their birth emotions, learn how to spot the signs and symptoms of any concerns, how and who to discuss these with. After all, it is their body-their recovery, they should know how.
Empowering mothers in the home setting is the very essence of what personalised care –supported self-management is. Whilst their post-partum recovery is not long-term their needs for a full recovery should include the opportunity to self-manage, so it follows that as health professionals we should arm them with the knowledge, tools, and skills to do this. Support for self-management is part of the shift in relationship between health and care professionals and people represented by personalised care.
Recommending, and sharing the details of this manual, is an investment of approaches to working with mothers and their support network based on their personal needs and individual assets. The authors have considered some inequalities, and accessibility barriers by providing valuable online links, to videos and internet pages of support, in order to create, a first of its kind recovery manual that is personalised and based on contents of ‘what matters’ to C-Section birthing mothers.
Our mantra has always been: ‘Once the stitches are in, the recovery begins….
Rastas L. McKnight-Cowan J., C-Section recovery manual: Your body, Your recovery 2022 Ocean Reeve Publishing https://www.waterstones.com/book/c-section-recovery-manual/leonie-rastas/janine-mcknight-cowan/9781922461957
Janine McKnight-Cowan BEM, BScHons Midwifery, BSc Hons Specialist Public Health Nursing (HV), Queens Nurse, Winner of 2019 RCNi Community & General Practice Nurse of the Year.
Currently Personalised Care Project Lead-Workforce Derbyshire Joined Up Care
Feb 2023