With current shortage of maternity staff in services stress and burnout continues to be high. Gina Finnerty, Visiting Fellow at the Institute for Lifecourse Development (ILD) at the University of Greenwich, discusses burnout and how this may be recognised and reduced in the workplace.
_________________________________________________
Introduction
This blog has a focus on occupational burnout because it is such a common phenomenon on the frontline in midwifery and maternity care. It has been suggested that burnout has become a silent epidemic that affects millions of people globally (Azzahra 2024). High levels of burnout in maternity care have inevitably affected quality of care and led to significant attrition of staff (Sidhu et al 2020). However, burnout can, in fact, be overcome as it is not usually permanent (Kendall-Tackett & Beck 2022).
Many of you are likely to have been affected to some degree, whether as midwives, managers, lecturers, maternity support workers, student midwives or doulas. Whatever your professional role in the maternity services, if you’ve been hit by fatigue caused by burnout, you are not to blame. Schaffer (2024) in her book ‘Exhausted’ cites lack of role clarity, minimal support, unrealistic workloads and poor communication in the workplace as key problems. It’s important to recognise early signs and symptoms (Soria et al 2024).
Firstly, the concept and broad definitions of burnout will be introduced. Secondly, the specific phases and characteristics of burnout will be shared. Finally, some specific solutions related to addressing burnout in maternity care settings will be suggested.
Definitions of burnout
The World Health Organisation (WHO)(2019), defines occupational burnout as a syndrome resulting from chronic work-related stress, with symptoms characterised by ‘feelings of energy depletion or exhaustion; increased mental distance from one’s job or feelings of negativism or cynicism related to one’s job; and reduced professional efficacy’’
In January 2025, ‘The Burnout Report’ was published by the charity, Mental Health UK. It is clearly written and presented. The report highlights the sobering fact that in the sample of 2060 adults surveyed, 35% expressed that they had experienced high or extreme work pressure in the past year. Significantly 20% had taken time off work due to stress and burnout. Brian Dow, the chief executive of Mental Health UK suggests that due such high levels of absence from work caused by poor mental health, a national summit on burnout is required.
Midwifery research studies (for example, the WHELM study (Hunter et al 2019), the POPPY study (Slade et al 2018) and the FUSCHIA cohort study (Matthews 2023) indicate that numbers of midwives experiencing burnout are significantly higher than in the average population. Robyn Matthews (2023) in fact found that 63% of midwives in Victoria, Australia had experienced work-related burnout. A high proportion of younger, early career midwives reported that their alcohol consumption had increased due to stress, and they had considered leaving the profession due to ‘having nothing left to give’.
What is the duty of care by managers? Jan Smith (2021) indicates that strong leadership is necessary to improve psychological safety and prevent PTSD and burnout in the workplace. There is no place for blame, shame or bullying. It is essential that workplace behaviours such as kindness, respect, trust and civility are visible when midwives are overwhelmed in clinical practice. What must be remembered is that we all entered the profession with the best intentions; to provide excellent safe, compassionate care to women, their babies and families.
Recognising burnout in yourself or your colleagues
Can you detect the signs and symptoms in your midwifery and maternity care colleagues?
In NHS midwifery practice, we need to understand the primary causes of burnout and how can it be spotted and managed well.
Inventories commonly used to assess levels of burnout are the Maslach Burnout Inventory and the Copenhagen Burnout Inventory. Both tools have different theoretical underpinnings. Sidhu et al (2021) undertook a comprehensive literature review on burnout in midwives and concluded that, due to linguistics, the Maslach inventory is less adaptable to diverse cultures. A specific Burnout Assessment Tool (BAT) for midwives was subsequently created in Sweden (Hadzibajramovic et al 2022). Midwives’ burnout levels were measured using four subscales:
- Exhaustion
- Mental distance
- Cognitive impairment
- Emotional impairment
Midwives and maternity staff who are neurodivergent are likely to experience burnout more profoundly. This is often due to the unpredictability and pressures of the workplace and also sensory overload (National Autistic Society 2024). I would suggest it is time to co-create a new burnout measurement tool with relevant stakeholders which is inclusive, relevant and fit for purpose in the current NHS.
Phases of burnout
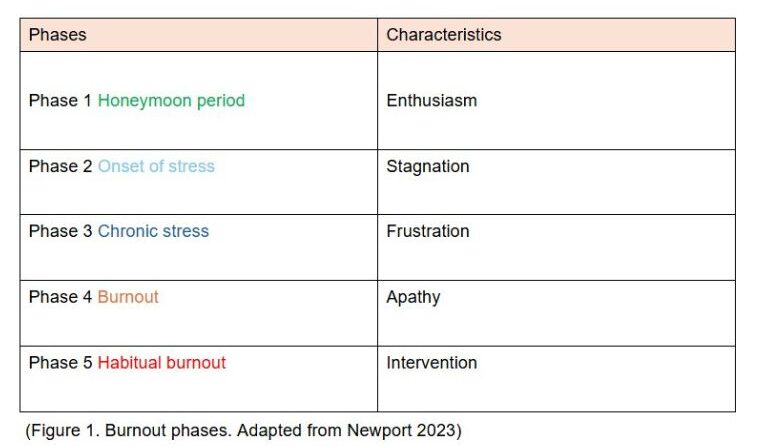
Cal Newport, an expert in workplace productivity in the US, has identified 5 distinct phases of burnout to look out for in your colleagues:
Wellness literature has burgeoned, and key headline advice is to engage in meditation, yoga, journalling, forest bathing etc and practise self-compassion to tackle occupational burnout. This is often totally unrealistic if working 12-hour shifts. The WHISPAs Network was launched in 2024 to examine wellness interventions in the workplace ( https://whispas.co.uk). Studies in the UK point to the disconnect between occupational health and human resources across all NHS professions. The cost of attrition from midwives leaving the NHS due to burnout and disillusionment indicates that meaningful engagement between occupational health and HR departments should be a priority to inform policy and practice.
Amity Reed (2020) describes being a survivor of severe burnout in her book, ‘Overdue’. She was an early career midwife who had previously had experience as a doula and enjoyed providing truly woman centred care. Due to lack of support in what she describes as a toxic culture, Amity left the NHS after only three years. Amity has contributed an excellent guest blog in a new website www.themasterfulmidwife.com, which details her troubling lived experience of burnout on the frontline.
Jennifer Moss (2020) has written a helpful article, advising that anyone experiencing more severe work-related burnout (eg phases 3-5, see Figure 1) should seek expert help and not rely on self-care. Moss’s argument is that, if burnout is hidden, the problem becomes minimised and reduces accountability for employers.
What can we learn from other professional groups to reduce burnout in the workplace?
- Occupational psychologists Evans and Steptoe-Warren (2019) suggest that compassion focused therapy has proved successful in dealing with trauma and burnout in the fire service.
- General Practitioners have reported positive results through initiation of a buddy system and monthly meetings to discuss mental health issues in general practice (Sinsky et al 2020)
- In neonatal nursing, the CORES model was used. This framework involves practical coping strategies involving Counselling, Open communication, Respite or time off following a traumatic event, Education to help cope with traumatic stress and Support from peers (Favrod et al 2018)
- Psychology staffing on the neonatal unit (ACPUK 2022). Employing a hub psychologist in NICU units was found to reduce burnout, PTSD and sickness/absence of staff. A psychologist presence has become more widespread in maternity care but should be standardised with a hub psychologist in every maternity unit. https://acpuk.org.uk/wp-content/uploads/2022/09/Psychology_Staffing_on_the_Neonatal_Unit.pdf
Suggested solutions in maternity care
- An enabling work environment (Feeley et al 2023) and an expansive learning environment through coaching models in maternity settings
- Adaptation of the Australian workplace culture tool; Empowerment in Midwifery Scale (Catling et al 2022)
- More trained Professional Midwifery Advocates to provide restorative supervision
- Dedicated Wellness Leads in every clinical area
- Formalised debriefing after every shift (Evans et al 2023)
- A refreshed approach to appraisals by managers, using positive peer review mechanisms and inclusive of a burnout inventory/burnout scale for each employee. Reasonable adjustments should then be tailored to each employee.
Conclusion
The literature related to burnout demonstrates that taking a holistic approach is essential. The purpose is to prevent burnout as far as possible but have robust systems in place if it does occur. Burnout inventories need to be adapted to be relevant to the current climate and experiences of NHS frontline maternity staff. If managers use the appraisal system more systematically, individual adjustments can be made. This will help staff to manage stress, to create boundaries and stay balanced. Ultimately, midwives and maternity staff are more likely to stay in the profession, feeling nurtured, resilient and able to flourish. Examining models of good practice and what works well in other professions could offer suggestions for increased work satisfaction and retention. Importantly, the knock-on effect will be improved care episodes for women, birthing people and babies. As Brian Dow (2025) suggests, a national summit on burnout could be transformative in escalating burnout as an important issue and contribute to the NHS Ten Year Plan agenda.
References and links
Azzahra S (2024) Invisible Burnout: The Hidden Epidemic in Modern Life and How to Overcome It. Format: Kindle Edition
Catling C, Rossiter C, Cummins A, McIntyre E (2022) Midwifery workplace culture in Sydney, Australia Women and Birth 25 (4) pp e379-e388
Evans T, Steptoe Warren G (2019) Applying Occupational Psychology to the Fire Service. Emotion, Risk and Decision-Making London: Springer Nature
Evans TR, Burns C, Essex R, Finnerty G et al (2023) A systematic scoping review on the evidence behind debriefing practices for the wellbeing/emotional outcomes of healthcare workers Frontiers in Psychiatry doi: https://doi.org/10.3389/fpsyt.2023.1078797
Favrod C, du Chene LJ, Soelch CM, et al (2018) Mental Health Symptoms and Work-Related Stressors in Hospital Midwives and NICU Nurses: A Mixed Methods Study Frontiers in Psychiatry doi: 10.3389/fpsyt.2018.00364
Feeley C (2023) Supporting Physiological Birth Choices in Midwifery Practice. The Role of Workplace Culture, Politics and Ethics. Oxford: Routledge
Greenstock K (2023) Flourish. A practical and emotional guidebook to thriving in midwifery London: Pinter and Martin
Hadzibajramovic E, Hansson M, Skerstrom M, et al (2022) Burnout among midwives-a factorial structure of the burnout assessment tool and an assessment of burnout levels in a Swedish national sample BMC Health Services Research 22:1167
Hunter B, Fenwick J, Sidebotham M, Henley J (2019) Midwives in the United Kingdom: Levels of burnout, depression, anxiety and stress and associated predictors Midwifery 79, 102526
Kendall-Tackett K, Beck C (2022) Secondary Traumatic Stress and Moral Injury in Maternity Care Providers: A Narrative and Exploratory Review. Frontiers in Global Women’s Health
Vol 3 https://doi.org/10.3389/fgwh.2022.835811
Matthews R (2023) Future-proofing the midwifery profession in Victoria: Sustainability, health and wellbeing of Victorian midwives. Australian College of Midwives 32 (1) 10-15
Mental Health UK (2025) The Burnout Report https://euc7zxtct58.exactdn.com/wp-content/uploads/2025/01/16142505/Mental-Health-UK_The-Burnout-Report-2025.pdf
Moss J (2020) Rethinking Burnout: When Self Care Is Not the Cure American Journal of Health Promotion 34 (5) https://doi.org/10.1177/0890117120920488b
Newport C (2023) How to recover from burnout. 20 steps. https://reclaim.ai/blog/how-to-recover-from-burnout#:~:text=Burnout%20is%20a%20stress%20response,activities%20that%20make%20you%20happy.
Reed A (2020) Overdue. Birth, burnout and a blueprint for a better NHS London: Pinter and Martin
Schaffner AK (2024) Exhausted. An A-Z for the Weary London: Profile Books
Sidhu R, Bowen S, Shapiro K, Stoll K (2020) Prevalence of and factors associated with burnout in midwifery: a scoping review European Journal of Midwifery 4 (4) doi.org/10.18332/ejm/115983
Sinsky C, Biddison LD, Mallick A, et al (2020) Organizational Evidence-Based and Promising Practices for Improving Clinician Well-Being NAM Perspectives doi: https://doi.org/10.31478/202011a
Slade P, Sheen K, Collinge S, et al (2018) A programme for the prevention of post-traumatic stress disorder in midwifery (POPPY): indications of effectiveness from a feasibility study European Journal of Psychotraumatology 9 (1):1518069. doi: https://doi.org/10.1080/20008198.2018.1518069
Smith J, (2021) ‘Nurturing Maternity Staff; How to tackle trauma, stress and burnout to create a positive working culture in the NHS’ London: Pinter & Martin
Soria J, Zervoulis K, Bolou A (2024) A survey examining the relationship between burnout, professional empowerment and personality traits of midwives of an inner London NHS Trust European Journal of Midwifery 8 (13)
World Health Organization (2019) Burnout an “occupational phenomenon”: International Classification of Diseases. Geneva: World Health Organization; 2019. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
Online resources:
An excellent resource, presented by a dynamic senior midwife. Trauma informed exercises and tips are presented in an accessible way to help you survive and flourish in your role.
This website, hosted by GPs, includes excellent webinars to reduce burnout, for example, on boundary setting and rest/sleep. There are links to, for example, a helpline- NHS Staff Emotional Support Service- (a free staff line for support, signposting and confidential listening and podcasts, such as moral injury.
3. https://www.wildmonday.co.uk/workwell
The aim of the website is to prevent burnout and also reduce sickness and workforce turnover. The mission is to improve staff resilience and retention. Sections have been devoted to support teams and to offer training and support for wellbeing leads in organisations. Many elements are directly transferable to health care but there is a cost for each module.
Author:
Gina Finnerty (PhD, B.Ed, RM) is a Visiting Fellow at the Institute for Lifecourse Development (ILD) at the University of Greenwich.
Gina is affiliated to the Centre for Professional Workforce Development and has launched a website in February 2025, The Masterful Midwife www.themasterfulmidwife.com. Restorative day retreats for frontline NHS midwives are being hosted in the New Forest, Hampshire, UK. Please use The Masterful Midwife website contact form to book a retreat.
March 2025


