This week the Maternity and Midwifery Forum’s Scotland Festival took place in Edinburgh. Dr Maria Pollard, Deputy Director NMAHP/Lead Midwife, and Tom McEwan, Head of Programme, NHS Education for Scotland spoke at the festival and in this article they share information on the National Midwifery Preceptorship Framework for Scotland.
_________________________________________________
Every newly qualified midwife in Scotland deserves a preceptorship experience that is structured, supportive, empowering and individualised to their learning and development needs. This framework provides guidance on how midwifery preceptorship should be planned, delivered and evaluated within an enabling environment. It is designed for newly qualified midwives, those new to the NMC register as a midwife, preceptors and service leads. It responds to recommendation 19 of the Midwifery Workforce and Education review (2021):
“A nationally agreed preceptorship programme should be developed for newly registered midwives, those returning to practice after re-joining the register or coming to work in the UK from within or outside the European Economic Area and European Union, and those in a new role”.
The framework represents feedback obtained through a national survey on current midwifery preceptorship practice and builds upon the principles and position statements of the Nursing and Midwifery Council (NMC) (revised 2022) and the Royal College of Midwives (RCM) (2022), and developed further by a national steering group. This framework also acknowledges and reflects much of the content from the First Five Years Forum (FFYF): Developing a preceptorship programme for newly qualified midwives in Scotland (2021) and RCM Preceptorship Guide (2023).
Within Scotland we have a TURAS Learn resource for Preceptorship (registration required to access) which provided the foundation for this framework. This generic framework was developed to support nurses, midwives and specialist community public health nurses (SCPHN) in their transition as newly qualified practitioners. In Scotland the concept of preceptorship has broadened to include nurses and midwives new to a role or environment, for example internationally recruited nurses or midwives, those who have transferred to a new ward or setting or who have secured a promotion and those new to managerial and executive roles.
Six Scottish standards were identified to support the implementation of the standalone midwifery preceptorship framework, as recommended by the Midwifery Workforce and Education Review, and builds upon the existing national generic preceptorship framework. These recognise many of the elements already included across NHS Board induction programmes and represent best practice (see Figure 1).

Figure 1- Scottish standards for midwifery preceptorship.
The midwifery preceptorship programme is flexible and designed with a 12–18-month timeline for completion in mind. The standards span the duration of the preceptorship programme and complement the six key components of the framework (see Figure 2), with a summary for each to follow. They support preceptee empowerment to influence their own preceptorship experience in partnership with their named preceptor recognising the knowledge, skills and attributes they currently possess.
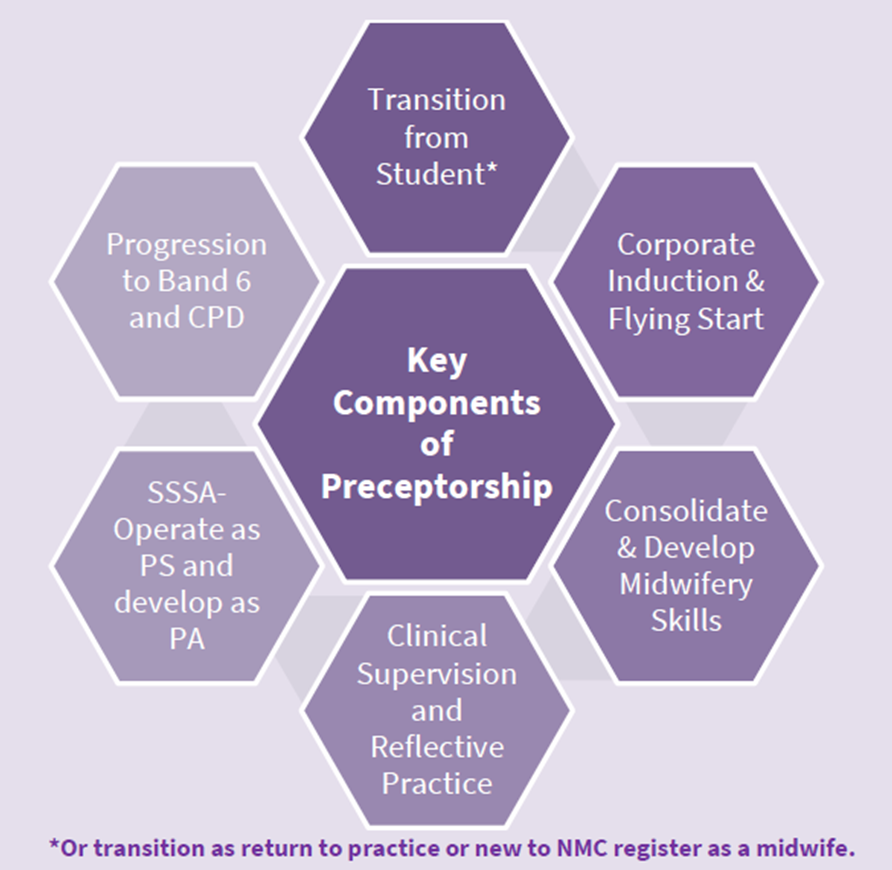
Figure 2- Key components of preceptorship.
The transition component is essential and provides the starting point for an individualised preceptorship experience for the newly qualified or new to NMC registration midwife. The conversations at this initial stage link to their induction, planning their clinical skills consolidation, preparation for band 6 progression, planning Continuous Professional Development (CPD) and reflection.
The next component reflects the extensive list of statutory and mandatory corporate training that employees within NHS Scotland Boards are required to complete, often during their induction, with some elements already included within pre-registration programmes. The duration for completion of these elements is not specified but suggestions that these are prioritised into time critical topics (e.g., fire safety, violence and aggression etc) and completed in the first 3-4 months with the remaining training completed by 12 months.
Flying Start NHS® is the national development programme for all newly qualified nurses, midwives and allied health professionals, to be undertaken and completed in the first year of practice. It combines individual learning with support in the workplace across the Four Pillars of Practice– clinical practice, facilitation of learning, leadership and evidence, research and development. It aims to support the preceptee to develop their confidence and skills, leadership ability, explore values and behaviours and make a positive start to their CPD.
The consolidate and develop midwifery skills component directly links to the individual learning needs identified in the early conversations between preceptee and preceptor, recognising the areas for their personal development. It is not a reassessment of skills already achieved and demonstrated for registration. Instead, it should support the practitioner to further enhance their confidence related to autonomy and advocacy as a new registrant, reflecting the philosophy of midwifery care, which is holistic, respectful, personalised, non-authoritarian and emancipatory. Traditionally preceptees have been offered a fixed rotation throughout key clinical areas in their employing NHS Board, supported with periods of supernumerary practice. This has been deemphasised within this framework to encourage the individual learning needs to be considered before an appropriate range of clinical experiences are offered for the purpose of consolidating their midwifery knowledge and skills.
Clinical Supervision is considered a priority for all midwives, with the foundation for this developed in the preceptorship period. It can take the form of Practice, Restorative or Professional Supervision. Midwifery specific guidance for clinical supervision in Scotland is currently under development. This component comprises the preceptee receiving regular clinical supervision whist completing their fundamentals of supervision online learning package. Furthermore, there is recognition of the midwife as a reflective practitioner and providing opportunities for the preceptee to capture this within their professional portfolio is actively encouraged.
Newly qualified midwives should be Practice Supervisor ready at point of registration. Those new to the NMC register may require additional support and training before undertaking the practice supervisor role. As such they should be supported in the first few months to act as a practice supervisor with support, progressing to an independent practice supervisor by midway in their first year of employment. Thereafter, and with the support of their preceptor and local Practice Education Facilitator (PEF), they can prepare for the Practice Assessor role.
Lastly, the preparation for progression to a Band 6 midwife is a key milestone. This framework advocates that this progression be outcomes based and not reliant solely on successful completion of the Flying Start NHS® programme. Personal Development Planning (PDP) and the appraisal process is initiated within the first month of employment, with goals identified as part of the individualised learning needs discussion. Preceptees should be introduced to the Band 6 job description at an early stage and encouraged to self-assess against these criteria for their PDP. Whilst many may be ready for this transition towards the end of their first 12 months of employment, others may require additional time to demonstrate evidence for this role development. The criteria in Figure 3 should be used by the line manager as the basis of an objective and outcomes focussed approach to transition from a Band 5 to Band 6 midwifery role.
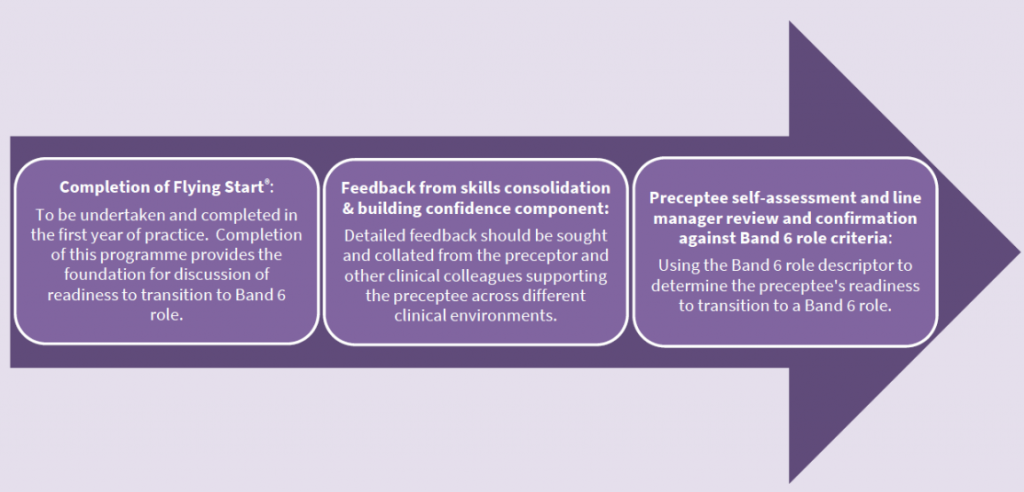
Figure 3- Transition to Band 6.
To support the ongoing implementation and evaluation of this framework an online survey link is embedded within the framework to gather ongoing feedback. In addition, five pathfinder NHS Boards in Scotland are working with NES to develop an evaluation approach for the first year of implementation which will include case studies comprising preceptor and preceptee dyads from each NHS Board.
We can, and must, do all we can to support those joining our profession and ensure they flourish and fulfil their future potential. We believe this framework provides the foundation and structure to realise this ambition.
Dr Maria Pollard, Deputy Director NMAHP/Lead Midwife, and Tom McEwan, Head of Programme, NHS Education for Scotland.
November 2023