The information on whether to have vaccinations during pregnancy and breastfeeding (or even breastfeeding when pregnant) is often confusing and frightening to women. As a result, women may refuse or feel forced into having the vaccination without full information. In this article Wendy Jones PhD MRPharmS MBE, pharmacist dispels some of the myths and points to resources to help midwives give the best information.
_______________________________
The long-term impact of the use of thalidomide for nausea in the 1960’s continues to be in the minds of many pregnant women and their families. They fear exposing their growing baby to anything from foods to medicines to passive smoking. The anti-vax campaign after COVID-19 still lurks when we discuss the benefits of vaccination in pregnancy. Women should not be dismissed but their fears acknowledged, and evidence-based information provided.
We can share with them that vaccination is recommended for Flu and COVID-19 as their own immunity is supressed in pregnancy making them more prone to infections which can be more severe than normal. In addition, no vaccination would be added to the schedule without significant consultation on risks and benefits by the UK Teratology Information Service. The vaccines are also given to protect the vulnerable newborn from infections and possible hospitalisation.
Active listening
As part of my training as a volunteer breastfeeding supporter I learned about active listening and how that can help someone clarify their fears, doubts and intentions. I have continued to use these in all areas of my professional practice and within the family!
These skills include:
- making eye contact, if possible (many of us, as healthcare professionals, are busy filling in forms and records as we talk!),
- picking up the non-verbal clues (how are they sitting, sounding?),
- not interrupting or phrasing the question with an implied agreement. For example, “so you are going to have the vaccine, aren’t you?” But maybe “at this stage in pregnancy we normally offer vaccine x, how do you feel about that? Do you have any questions?”
- unconditional respect for that decision, we are not in a position to judge. You could offer further information for the family to look at and discuss. Written information is powerful. Think how many people believe everything they find on google searches! Ensure that you are providing appropriate evidence-based information.
- show that you are listening by nodding and don’t pass on your opinions.
- paraphrase back to the family the concerns that they might have expressed. “So, I’m hearing that you have seen some experiences and opinions on social media that are concerning you. Is that correct?”
- ask open questions rather than anything to which the expected reply is yes or no.
We cannot force vaccinations onto pregnant women without addressing their concerns, if they have them. Otherwise, they may worry for the rest of the pregnancy that they have damaged this precious baby which may not have been conceived simply and on who great hopes are placed. NICE has particularly emphasised that all healthcare professionals should be facilitating shared patient choses in all aspects of their care.
The vaccinations recommended in pregnancy are currently Flu, COVID-19, Whooping Cough, Respiratory syncytial virus (RSV) vaccine.
Flu vaccine
Flu vaccination is recommended in pregnancy to protect the woman from complications of flu and to help prevent the baby from catching flu in the first few weeks after delivery. Pregnant women are more likely to suffer complications such as chest infections and pneumonia. https://www.medicinesinpregnancy.org/leaflets-a-z/flu-vaccine/
Whooping Cough vaccine
The whooping cough vaccine is given sometime after 16 weeks but normally around 20 weeks. Some immunity passes across the placenta protecting the neonate until it can have its own vaccination. There has been an increase in cases of whooping cough reported over the past year and the youngest babies are at greater risk of severe illness and hospitalisation. There are sadly even reports of infant death. https://www.medicinesinpregnancy.org/leaflets-a-z/whooping-cough-vaccine/
Respiratory syncytial virus (RSV) vaccine
The new RSV vaccine given to the mother (available from 1.9.24) protects the baby for the first 6 months after birth from severe lung infections which may make it difficult for babies to breathe and necessitate hospital admission. The vaccine is normally offered around 28 weeks of pregnancy. RSV is a common virus that causes coughs and colds but can lead to bronchiolitis in babies making it difficult for them to breathe and feed. https://www.gov.uk/government/publications/respiratory-syncytial-virus-rsv-maternal-vaccination/a-guide-to-rsv-vaccination-for-pregnant-women
COVID-19 vaccine
The COVID-19 vaccine can be given at any stage in pregnancy. It protects both mother and baby. Pregnant mothers who develop COVID-19 can become seriously ill. If the mother contracts it late in pregnancy the baby may become seriously unwell and need to be admitted to special care.
https://www.medicinesinpregnancy.org/leaflets-a-z/covid-19-vaccine/
Live virus vaccines
Vaccines to be avoided in pregnancy include all those which contain live virus. These include MMR, BCG and Oral typhoid, polio and yellow fever
Vaccination during breastfeeding
Breastfeeding mothers can have all routine vaccinations which they may have missed, and which are injected e.g. MMR, Flu, COVID-19.
The vaccines are not transmitted through breastmilk as they are poorly orally bioavailable and so cannot be absorbed from breastmilk. Healthcare workers can receive hepatitis vaccines without interrupting breastfeeding.
Other vaccines which can be used are chickenpox, hepatitis a and c, pneumonia, tetanus, typhoid, BCG, DipPT, whooping cough, injected polio vaccine (but not oral drops).
Children’s vaccines which can affect the mother.
Immunocompromised mothers i.e. those taking drugs such as azathioprine, biological drugs (Infliximab, Humira™ etc) should wear gloves when changing nappies for 2 weeks if their baby is given rotavirus drops as part of their routine immunisation. This is because live viral particles are shed in faeces for two weeks. https://breastfeeding-and-medication.co.uk/fact-sheet/live-vaccinations-and-immunosuppressant-medication-taken-by-breastfeeding-mothers
Immunotherapy drugs given during pregnancy.
If the mother continued biological drugs during pregnancy the baby should not receive the rotavirus drops for at least 6 months (12 months for infliximab). This is because sufficient of the drugs pass the placenta to impact on the baby’s immunity. Other vaccines to avoid are BCG if that is necessary because the baby is at increased risk of contracting tuberculosis. https://www.nhs.uk/vaccinations/bcg-vaccine-for-tuberculosis-tb/
Although MMR vaccine contains a live virus there is little evidence of risk to an immunocompromised mother.
The card below was developed by Lorna Orriss-Dib at Healthwatch Essex as a resource for mothers with Inflammatory Bowel Disease to be stuck into the Red Book. Some healthcare professionals were not aware of the risks to women taking medication which caused them to be immunocompromised during pregnancy or when their babies received live vaccines, according to a study undertaken by Lorna. I have also witnessed this on the Facebook group which I administer for breastfeeding mothers with IBD. The card was developed as a simple tool to be ensure everyone was fully informed of the risks and benefits. Healthwatch Essex are keen that it can be widely disseminated to other areas.
The information applies whether the mother is breastfeeding or using infant formula if she is immunocompromised.
In summary:
- For mothers who were taking biological medication in the third trimester of pregnancy, their babies, should not receive live vaccinations before at least 6 months of age
- Mothers who are immunocompromised may be infected by faecal particles shed following the use of rotavirus vaccine to their baby and should take hygiene precautions
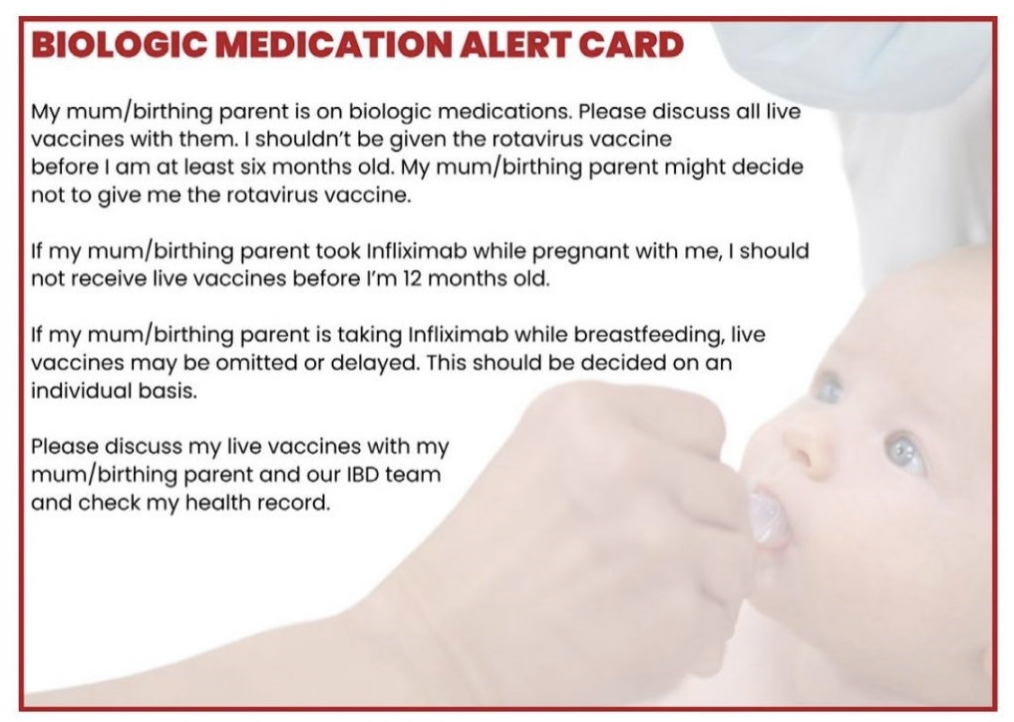 Image developed by Lorna Orriss-Dib at Healthwatch Essex. Reproduced with consent and can be widely disseminated).
Image developed by Lorna Orriss-Dib at Healthwatch Essex. Reproduced with consent and can be widely disseminated).
Further information
Breastfeeding and Medication https://breastfeeding-and-medication.co.uk/fact-sheet/vaccines-and-breastfeeding
Immunisation against infectious disease. The Green Book https://www.gov.uk/government/collections/immunisation-against-infectious-disease-the-green-book
Kroger AT, Atkinson WL, Marcuse EK, Pickering LK, Advisory Committee on Immunization Practices (ACIP) Centers for Disease Control and Prevention (CDC). General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP), MMWR Recomm Rep, 2006;55(RR-15):1–48.
Plotkin SA, Orenstein WA, Vaccines 4th edition, Philadelphia: WB Saunders, 2004 (cited in Department of Health Green Book chapter 34).
Using vaccines during breastfeeding https://www.nhs.uk/vaccinations/bcg-vaccine-for-tuberculosis-tb/
Vaccines in pregnancy Public Health Scotland https://www.youtube.com/watch?v=yqGN2tivZT4
UK Teratology Information Service. https://uktis.org/
NICE Shared Decision Making www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-guidelines/shared-decision-making
Wendy Jones PhD MRPharmS MBE
November 2024
To contact Wendy email wendy@breastfeeding-and-medication.co.uk



1 comment
I work in Essex and have never seen the alert sticker in a red book. What a shame, I know that in all this time I have met women with IBD etc. Very helpful article thanks
Comments are closed.