May is Ehlers-Danlos Syndrome Awareness month. It is a condition that may affect a significant number of people considering pregnancy. Dr Sally Pezaro, Assistant Professor (Research), Centre for Healthcare and Communities, Coventry university, and an international research team, have been working on new guidelines for pregnancy to help support those with this condition. She shares the information below.
__________________________________________________________________
An international team of experts, in collaboration with patients and advocates, has developed the first comprehensive guidelines for managing pregnancy, childbirth, and postpartum recovery in individuals with hypermobile Ehlers-Danlos syndrome (hEDS) and hypermobility spectrum disorders (HSD). This groundbreaking work represents a significant step forward in addressing the unique challenges faced by this population during their childbearing years.
The development of these guidelines was led by midwife, Dr Sally Pezaro, and supported by the Ehlers-Danlos Society. A total of 15 co-creators joined in meeting the aim of this research from the United Kingdom, United States of America, Canada, France, and the Netherlands. Co-creators represented a variety of professions including midwifery, obstetrics, maternal fetal medicine, rheumatology, registered dietitians, and nutritionists, physical therapy, clinical geneticists, nursing, clinical research, and pain management. Co-creators also included patient advocates with lived experience of both hEDS/HSD and childbearing. All are listed as co-authors to the final output:
Sally Pezaro, Isabelle Brock, Maggie Buckley, Sarahann Callaway, Serwet Demirdas, Alan Hakim, Cheryl Harris, Carole High Gross, Megan Karanfil, Isabelle Le Ray, Laura McGillis, Bonnie Nasar, Melissa Russo, Lorna Ryan, Natalie Blagowidow (2024) Management of childbearing with hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorders: A scoping review and expert co-creation of evidence-based clinical guidelines. PLoS ONE 19(5): e0302401. https://doi.org/10.1371/journal.pone.0302401
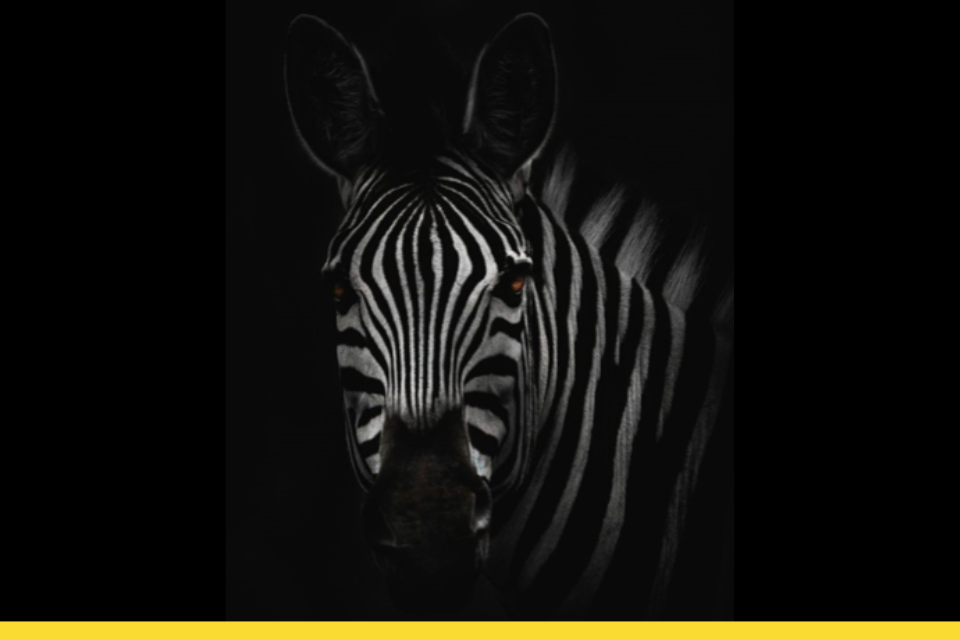
Ehlers-Danlos Syndromes (EDS) are often associated with zebras due to a common medical teaching phrase: “When you hear hoofbeats, think horses, not zebras.” This phrase encourages medical students and practitioners to prioritize common diagnoses over rare ones when evaluating patients. Whilst many types of EDS are rare, our research outlines how hypermobile EDS may affect up to 1 in 20 pregnancies, and simply be rarely diagnosed.

Understanding hEDS/HSD and Their Impact on Childbearing
hEDS and HSD are heritable connective tissue disorders characterized by joint hypermobility, tissue fragility, and other symptoms. These conditions can lead to various complications during pregnancy and childbirth, including:
- Increased bleeding due to fragile capillaries and potential blood clotting issues
- Joint instability and pain, exacerbated by pregnancy hormones
- Increased risk of pelvic organ prolapse and other pelvic floor issues
- Comorbidities such as dysautonomia, mast cell disorders, and spinal instability
A Collaborative Approach to Guideline Development
Recognising the complexity of these conditions and the importance of patient perspectives, the guidelines were developed through a multi-faceted approach:
- Scoping Review: A comprehensive review of existing literature on hEDS/HSD and childbearing provided a foundation of evidence.
- Expert Co-creation: A multidisciplinary team of healthcare professionals, including obstetricians, midwives, rheumatologists, geneticists, and others, evaluated the evidence and contributed their clinical expertise.
- Patient and Public Involvement (PPI): Individuals with lived experience of hEDS/HSD and childbirth actively participated in shaping the guidelines through conferences, online forums, and newsletters. Their invaluable insights ensured the final recommendations were truly patient-centred.
Comprehensive Guidance for All Stages of Childbearing
The resulting guidelines offer detailed recommendations for every stage of the childbearing journey:
- Preconception: Counselling and screening for potential risks and complications
- Antenatal: Risk assessment, management of miscarriage and termination, mobility support, and addressing comorbidities
- Intrapartum: Birth choices, pain management options, mode of birth considerations, and labour support
- Postpartum: Wound healing, pelvic health, newborn care, and breastfeeding support
- Additional Considerations: Guidance on pain management, mental health support, nutrition, and overall well-being
Key Recommendations and Insights
The guidelines emphasize the importance of individualized care, recognizing that each person’s experience with hEDS/HSD is unique. A multidisciplinary team approach is recommended to address the diverse needs of these individuals.
Key recommendations include:
- Early and ongoing risk assessment throughout pregnancy
- Individualized birth plans that consider the person’s specific needs and preferences
- Close monitoring for potential complications like bleeding and joint instability
- Proactive management of comorbidities
- Comprehensive postpartum care, including pelvic floor rehabilitation and infant feeding support
Looking Ahead: Further Research and Collaboration
While these guidelines represent a significant step forward, the authors acknowledge the need for further research to address gaps in knowledge and improve care for individuals with hEDS/HSD. Future studies should focus on the long-term effects of hEDS/HSD on pregnancy outcomes and the efficacy of different interventions.
Additionally, ongoing collaboration between healthcare providers, researchers, and childbearing people will be crucial for refining these guidelines and ensuring they remain relevant and responsive to the evolving needs of this population.
It is particularly exciting to have these guidelines published during Ehlers-Danlos Syndrome awareness month. – #TogetherWeDazzle
Conclusion
The development of these comprehensive, evidence-based, and person-centred guidelines marks a new era in the care of pregnant individuals with hEDS/HSD. By empowering healthcare providers with knowledge and fostering a collaborative approach, these guidelines have the potential to significantly improve outcomes for childbearing people and their babies.
You can read the full guidance here
Find out more via www.hEDSTogether.com.
We would be keen to hear how these guidelines are being used in practice and how they are making an impact in the real world. If you have an impact story, please get in touch.
Dr Sally Pezaro PhD MSc BA (Hons) PgCAPHE FRCM SFHEA RM
Assistant Professor (Research), Centre for Healthcare and Communities, Coventry university
May 2024


2 comments
I think it would also be good to look out for signs of EDS patients may not have noticed. I wasn’t diagnosed until 40. Had awful complications with my pregnancies/birth including severe hip separation, primary and secondary haemorrhage. Maybe patients presenting with joint complications could be screened or atleast signposted to information on EDS/hypermobility.
These new hEDS guidelines seem inadequate – pregnancy can be life threatening. I don’t see any guidance on this.
Our daughter nearly died during both her pregnancies – the first before she was diagnosed with hEDS, and the second after her first pregnancy complications led to her hEDS diagnosis very early in her second pregnancy.
At her first pregnancy pre-eclampsia and other complications were so great that she underwent a caesarian at 26 weeks gestation and her baby daughter was born 1lb 4oz – both needed hospital medical care for 14 weeks and both survived – thank you QMC.
From the start of her second pregnancy she was treateed as high risk – fortunately all the various Consultants involved in saving her life during and after her first pregnancy were still at QMC, so treating her for her second pregnancy, so none had to be educated on how life threatening that pregnancy was. They only had to learn about her having had to have had an ankle joint surgical repair a year and a quarter after her first pregnancy – having worn out her hypermobile ankle. This was not helped with continued relaxen hormone whilst pumping breast milk for her tiny daughter.
These amazing Consultants managed to stretch this second pregnancy to 32 weeks, when again a caesarian was performed to save her life, and her baby boy was born 3lb 3oz.
Both children have hEDS – in more severe forms than our daughter did in childhood.
Comments are closed.